Author:
Edward Brown, ST5,Freeman Hospital, The Newcastle-upon-Tyne Hospitals NHS Foundation Trust
Acknowledgments:
Dr Preya Patel, Consultant Hepatologist
Dr Aaron Wetten, Consultant Hepatologist
Dr Laura Jopson, Consultant Hepatologist
The rising rates of steatotic liver disease has resulted in an increasing number of patients requiring fibrosis assessment in secondary care. Locally the referral rate in 2023/2024 has increased by 93% in comparison to 2019/2020 from 2,566 to 4,964. Prior to the initiation of the intervention the compliance with the Referral to treatment Time (RTT) pathway was low at 68% and the average waiting time for a routine Hepatology outpatient review was approximately 9 months.
In response to this the “Direct to Fibroscan® Pathway (DTFP)” was introduced to assess and screen patients who have been referred by their GP with suspected fatty liver disease and identify those requiring a Hepatology clinic review. Referral letters from Primary Care to the Hepatology department were triaged by a Hepatology consultant. Patients with suspected fatty liver disease were triaged onto the DTFP. Patients triaged to the DTFP underwent a Fibroscan® performed by one of the Hepatology departments Fibroscan® technicians who had undergone brief intervention training to provide targeted advice related to diet, exercise, smoking and alcohol misuse. Data was collected prospectively on all patients referred to the DTFP.
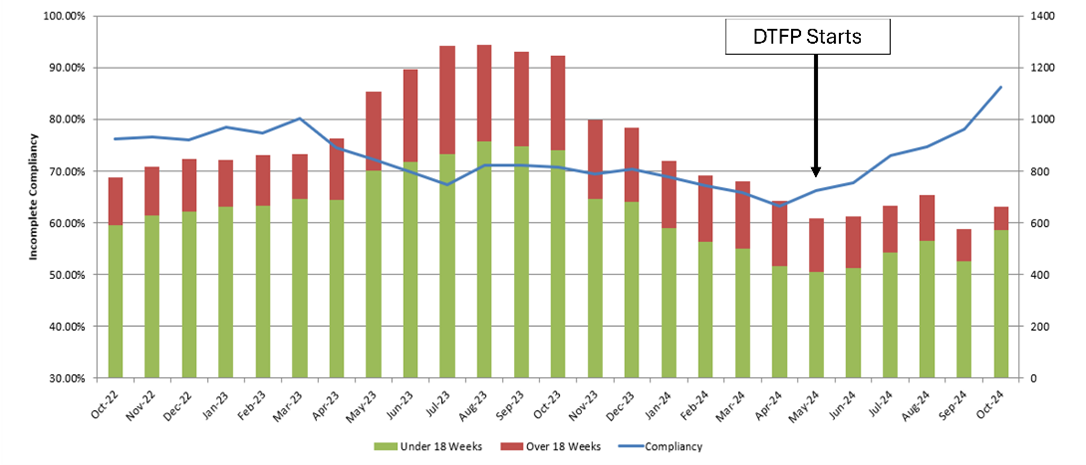
215 patients were triaged to the DTFP between 19/06/2024 and 11/12/24. GP’s were encouraged to calculate a Fib-4 score in order to help triaging. Patients that were triaged onto this pathway were invited for a Fibroscan® to assess if they had potentially significant fibrosis requiring further assessment (median liver stiffness >8kPa). Of the 215 patients invited for a Fibroscan® 163 (76%) attended for their appointment. Of these 163 patients 45 patients had a Fibroscan® result of >8kPa or had an invalid result and so were offered a Hepatology clinic appointment. The remaining 118 patients who had a Fibroscan® result of <8kPa were directly discharged from the pathway back to their GP with both lifestyle advice as well as re-referral criteria and monitoring advice for the GP (Figure 1). These changes have allowed for better utilisation of Hepatology outpatient clinic appointments which have aided in lowering waiting times and resulted in a significant improvement in the RTT 18 week compliance; which increased from 68.9% to 88% (p<0.001) 6 months after the implementation of the Direct to Fibroscan® pathway (Figure 2).
Introduction of this pathway has resulted in improved outpatient appointment waiting times for patients whilst identifying patients who are in greatest need of Hepatology input. Implementation of this pathway resulted in better utilisation of Hepatology outpatient appointments. Patients discharged directly from the DTFP were provided with lifestyle advice and basic interventions relating to alcohol misuse to modify their risk factors to prevent further deterioration in their liver health. Greater utilisation of Fib-4 scoring by GP’s could help to further streamline this referral service as an initial screening tool to highlight patients that potentially have significant liver fibrosis. Implementation of this pathway by other teams could result in improved efficiency in triaging of routine outpatient Hepatology appointments. This is a low-cost intervention that has shown to significantly improve RTT as well as still providing patients that are potentially at risk of significant liver fibrosis with appropriate targeted health education.
Figure 1: Flow chart of patients triaged to the DTFP.
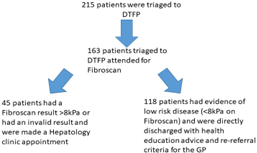
Figure 2: RTT performance before and after implementation of the DTFP. Expected standard is 92% patients begin treatment within 18 weeks of referral.
Read More

