BSG CSSC Service Development Prize 2023 highly commended submission by Dr Jaimik Patel
Names of team involved: Jaimik Patel, Anupama de Silva, Norfolk and Norwich University Hospital
What was the challenge?
Treatment pathway delays were identified in patients referred to the Colorectal Surgical Team under a lower GI cancer 2-week-wait pathway, who were subsequently found to have a new diagnosis of IBD made at colonoscopy. A retrospective audit from June to July 2021 revealed 25 patients with a new diagnosis of IBD made at colonoscopy. Only 9/25 (36%) patients were started on treatment on the same day as their colonoscopy. The average time taken to be seen in clinic was 106 days. 2 patients in this cohort required hospital admissions for IBD-related complications whilst awaiting clinic review. Delays were leaving patients on no, or sub-optimal, treatment and, in some cases, requiring hospital admission.
Improvement Strategy
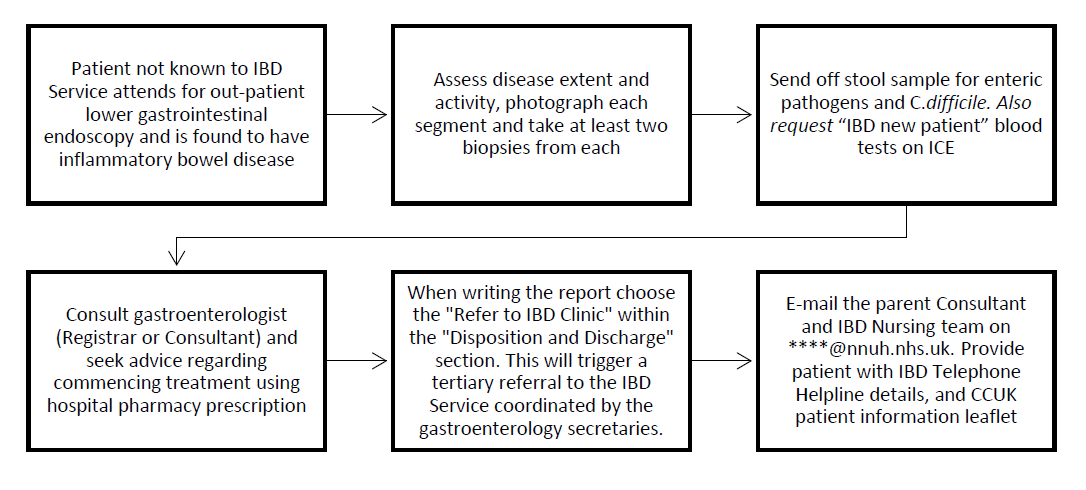
Early assessment and prompt treatment of newly diagnosed IBD is essential to improve symptoms and prevent adverse outcomes. A standard operation procedure (SOP) was written and implemented to guide endoscopists in assessing severity, starting treatment, and triggering an internal tertiary referral for patients with a first diagnosis of IBD to be reviewed at the next available IBD clinic with the consultant with the shortest waiting list (see fig 1.1).
Fig 1.1- Quick Reference Guide to SOP
.png)
Introduction of SOP
The SOP was initiated in December 2021 and during the initial 3 months, 26 patients with a new diagnosis of IBD at colonoscopy were audited to assess its efficacy and compliance. 12/26 (46%) patients were started on treatment on the same day, and 13/26 (50%) patients were successfully referred directly to the IBD Clinic from the Endoscopy Unit. The cohort of patients who triggered an internal referral to the IBD Clinic had, on average, a 28-day shorter waiting time to be seen in clinic as opposed to those referred through alternative routes.
Non-compliance with the SOP was found to be highest amongst surgical and outsourced endoscopists. Investigation into delays in the internal referral pathways revealed that some secretaries were delaying booking patients into the next available clinic slot, instead waiting for histology results to be available. It became apparent that knowledge of the SOP needed to be promoted to all clinical and non-clinical members of staff within the department to facilitate further improvement. As a result, the SOP was presented at the IBD Business Meeting, Gastroenterology Clinical Governance Meeting and Endoscopy User Group Meeting. Moreover, as we identified that a certain cohort of endoscopists were less likely to attend such governance meetings, a letter was sent out to all medical, surgical and nurse endoscopists informing them of the SOP and encouraging its use. Meetings with secretarial staff were held to highlight and prevent delays in the pathway. Senior Nurse Endoscopists were tasked with reviewing colonoscopy reports from procedures carried out by outsourced endoscopists to ensure patients with a new diagnosis of IBD had been correctly managed.
Outcomes
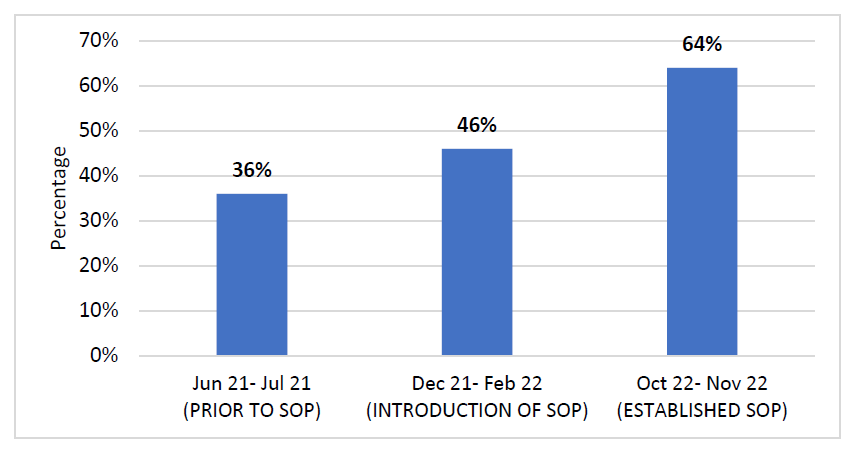
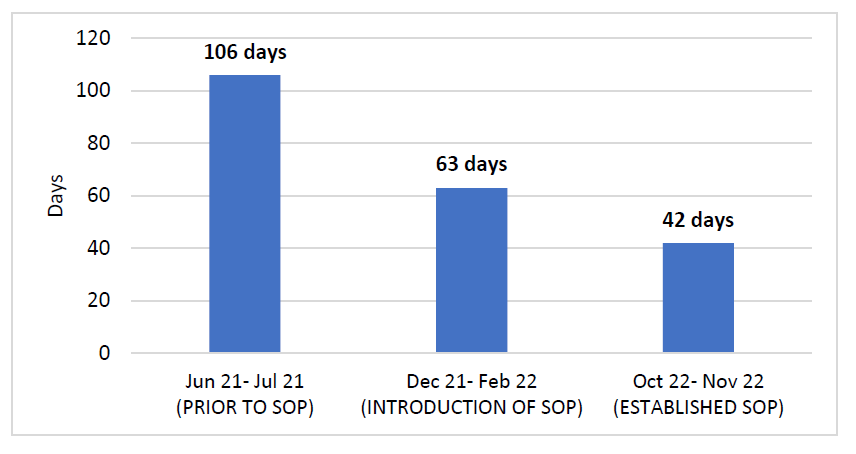
Approximately one year after the introduction of the SOP, treatment and waiting times of 25 patients with new diagnosis IBD were audited between October and November 2022. The proportion of patients prescribed treatment on the same day as their colonoscopy had increased to 16/25 (64%) from 9/25 (36%) prior to the SOP (see fig 1.2). Moreover, 18/25 (70%) patients were successfully referred directly to IBD clinic via the SOP pathway after their diagnosis at endoscopy. As a result, the average waiting time for an IBD Clinic review reduced to from 106 days to 42 days (see fig 1.3). No patients were admitted to hospital whilst awaiting their clinic appointment following their diagnosis of IBD at endoscopy.
Fig 1.2 Percentage of patients prescribed IBD treatment on the same day as endoscopy
.png)
Fig 1.3 Average waiting time to be seen in IBD clinic after first diagnosis at endoscopy
Conclusions/ Learning Points
- Patients with change in bowel habit and FIT-positivity referred to the Colorectal Team as a Lower GI Cancer 2-week-wait referral can reveal a new diagnosis of IBD
- Early assessment and prompt treatment of newly diagnosed IBD improves symptoms and prevents adverse outcomes
- Implementing and adhering to an SOP can be challenging within a large department with multiple sub-specialists working together to provide patient care
- Perseverance in promoting an SOP improves patient outcomes by facilitating prompt treatment and reducing clinic waiting times
Read More

