Authors:
A Pradeep, M Coles, K Dela Cruz, T Recato Dy, S Coate, K Mercer
Institute of liver Studies, Kings College Hospital, London
Role of Liver Transplant Recipient Coordinator
Introduction:
A liver transplant is a lifesaving operation for patients with end stage liver disease, involving removal of the diseased liver and replacement with healthy liver from either a deceased or living donor. The first liver transplant in the United Kingdom took place in 1968 and numbers of operations continue to grow year on year, with NHS Blood and Transplant recording close to 800 adult transplants taking place across 7 centres in 2024.
The Liver Transplant Coordinator (LTPC) is a clinical nurse specialist with autonomous and critical thinking skills, who plays an integral role within the multidisciplinary team looking after patients with liver disease. The LTPC supports both the patient and their family during all phases of the transplant process which include pre assessment, waiting list management, and the transplant, immediate and long term post-transplant care. Transplantation is a 24 hour service running 365 days per year, and as such, many complex decisions are made out of hours. It is an incredibly rewarding role where no 2 days are the same and the opportunities to develop autonomous practice are vast. This article reflect on some of the key aspects and clinical skills (Table 1) required in the LTPC role.
Table1: LTPC’s Essential Clinical Skills:
Table1: LTPC’s Essential Clinical Skills:
|
Key roles/responsibilities:
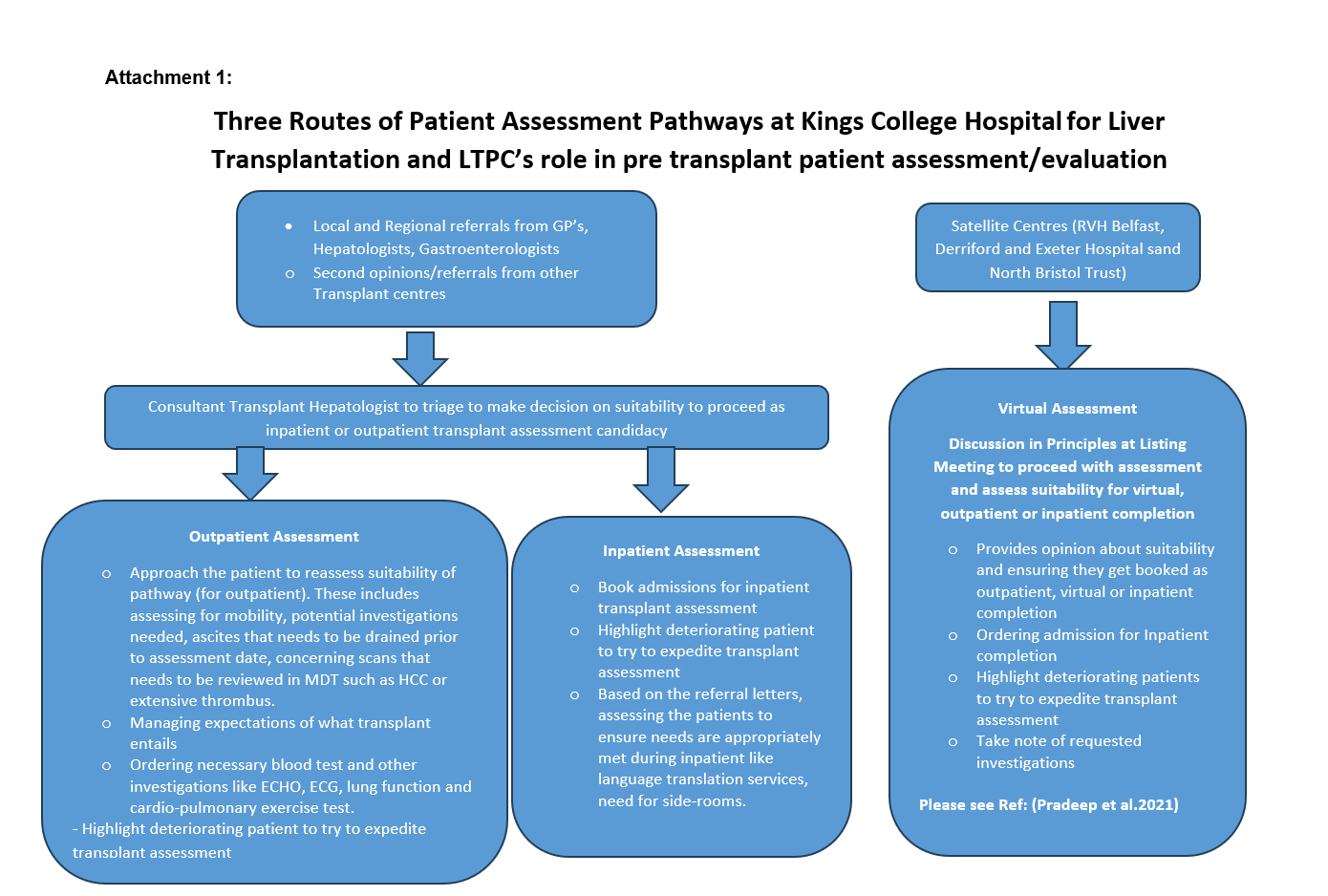
1. Assessment and Evaluation of Transplant Candidates:
Following the receipt of initial referral LTPC’s conduct comprehensive, holistic assessments to determine patients suitability for transplant including eligibility for NHS care. See attached flow chart explaining the assessment pathways and process (Attachment 1).
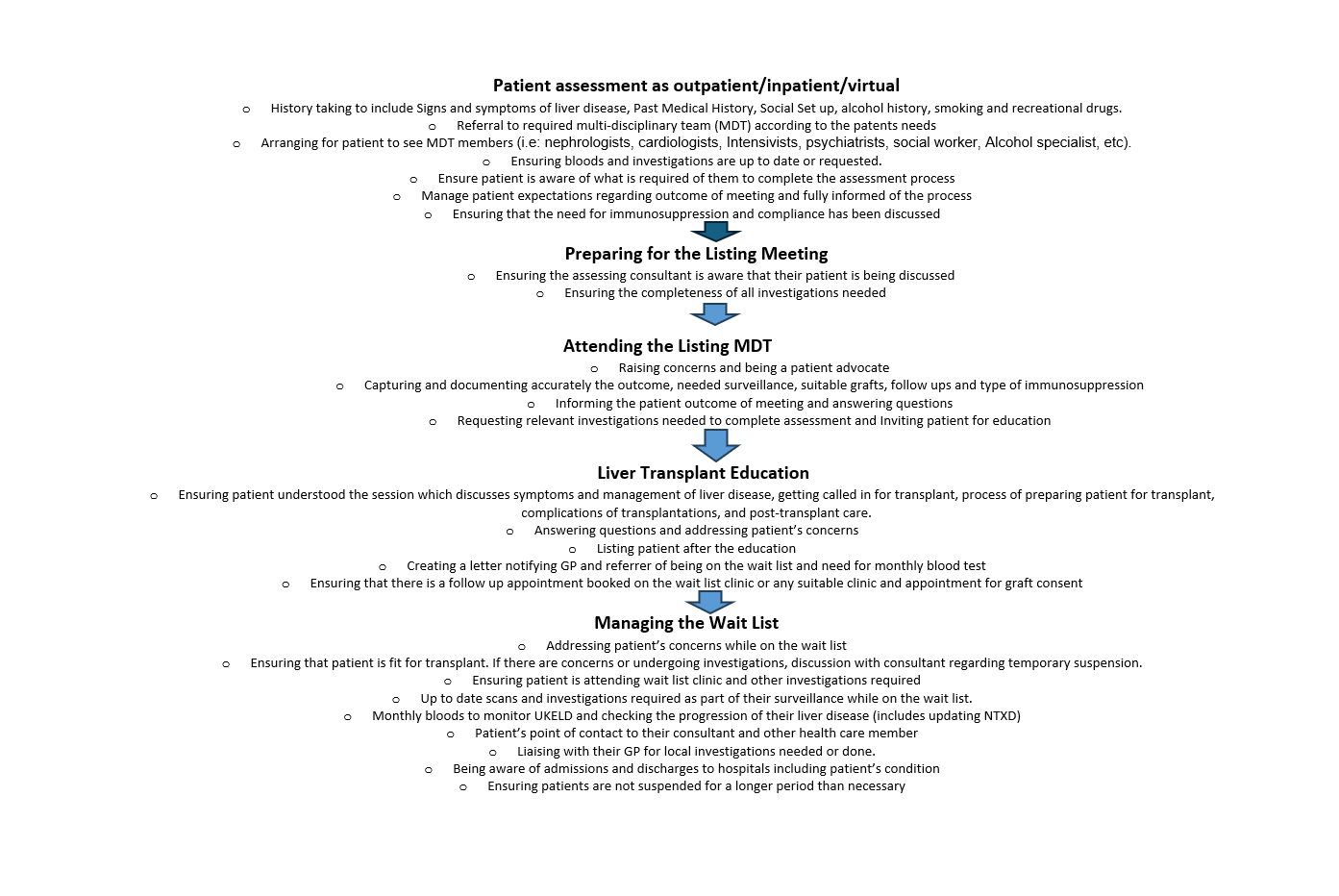
2. Patient Education and Support:
Educate patients and their families about the transplants listing process, waiting list management, call up process, transplant procedure, post-operative expectations, lifestyle modifications, and the lifelong commitment to anti-rejection and its side-effects and post-transplant complications. Offer psychological, emotional and social worker support (Attachment 1).
3. Patient Advocacy and Support:
LTPC remain as patients advocate to facilitate patient’s best interests within the healthcare system, ensuring they receive timely, effective, and respectful care.
Signpost and empower patients and families to access additional support resources, such as financial assistance, counselling, and patient support groups. Act as a mediator between patients and healthcare providers, helping to navigate any misunderstandings/conflicts regarding treatment and expectations.
4. Management of Transplant waiting period:
LTPC’s remain as the patient’s and family’s first point of contact during their transplant journey. Oversees the entire process once a patient is accepted onto the transplant waiting list. LTPC’s maintain the patients transplant status on local/national transplant waiting list and submit regular updates on patient’s clinical status which directly impacts on patient’s transplant benefits score, which plays a key role in organ allocation and potential opportunity for patients to receive a named organ offer. Follow up on radiologic imaging for those with tumours and vascular thrombus concerns. Monitor for appropriate vaccinations, and sign post the families to living donor coordinator accordingly. LTPC act as the central coordinator for communication, ensuring that transplant team are up-to-date on the patient’s status, needs, and changes in care plans.
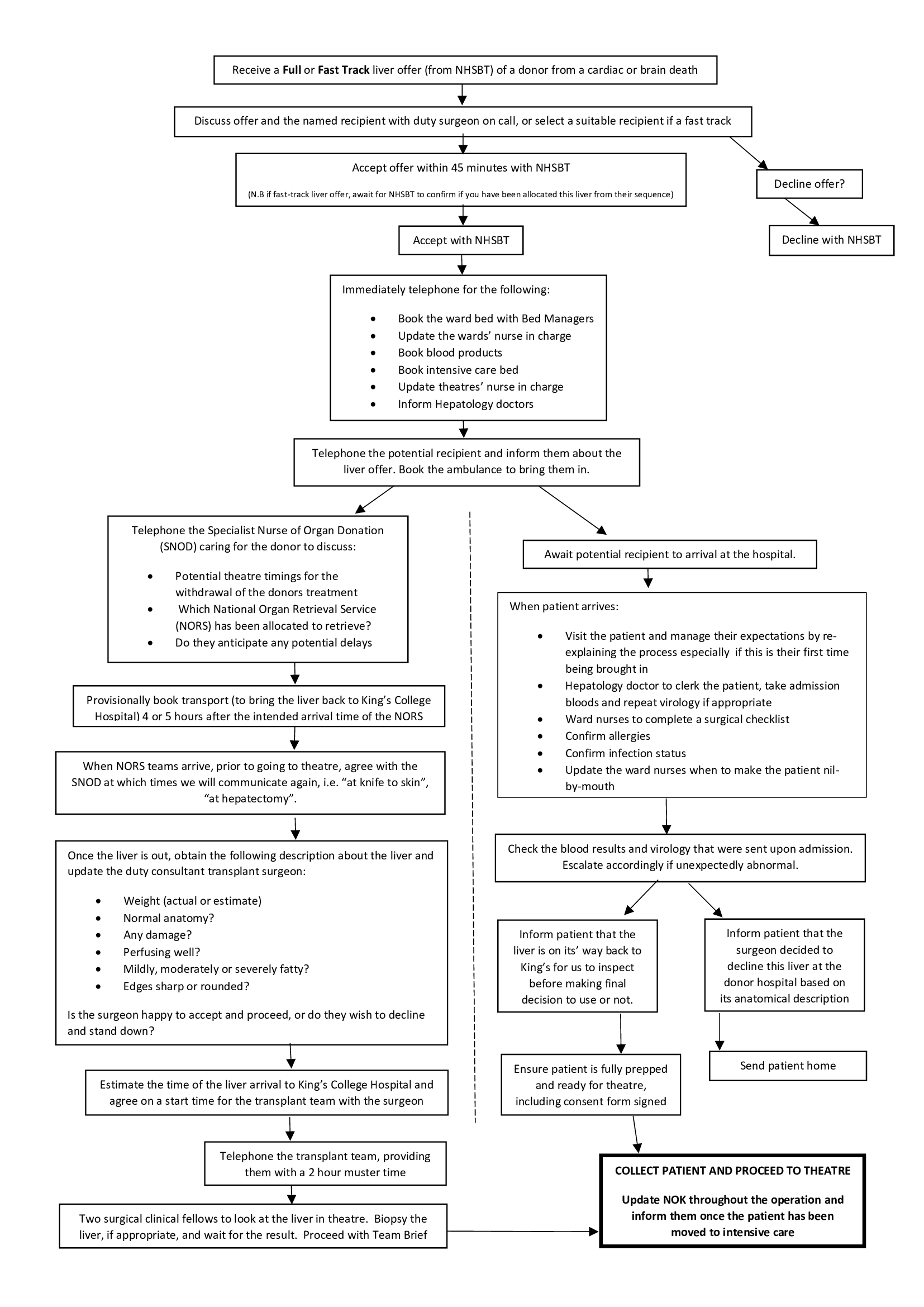
5. Coordination of the Transplant Process:
LTPC’s key role includes 24 hour on-call service to facilitate transplant activities: including contacting the potential recipient and manage the logistics of organ allocation and retrieval, liaising with Organ Donor and Transplant (ODT) Hub, Specialist Nurses for Organ Donation (SNOD’s), National Organ Retrieval Service team transplanting surgeon, and the operating theatre staff to plan the time of retrieval and transplant. Also, take a lead role in registering patients with acute liver failure for the super-urgent listing, ensuring they receive timely and appropriate care. This involves support and education of relatives and loved ones in a very acute environment. See attached flow chart explaining LTPC’s oncall responsibilities
6. Post-Transplant Care and Follow-Up:
Provide tailored education on self-medication and post-transplant discharge care. Monitor any donor related risk factors and notify the Clinicians/Microbiologists of any updates received from the SNOD’s. Report any adverse events to ODT and comply with local clinical governance policy. Post discharge, monitor through virtual clinics and remain the point of contact for patients and families. See attached flow chart explaining LTPC’s role in post-transplant care.

7. Documentation and Data Management:
Maintain accurate, thorough documentation of all stages of the transplant process, ensuring compliance with NHS policies, GDPR, Transplant regulatory standards and HTA requirements. Record and monitor clinical data, including pre and post-operative tests, patient progress, and long-term outcomes, to contribute to transplant quality and safety improvement programs. Ensure data entry into transplant registries and databases, analysis, and evaluation of transplant outcomes.
8. Policy Compliance and Quality Improvement:
Adhere to NHS and regulatory standards, ensuring safe and ethical practices in patient assessment, organ allocation, and follow-up care. Participate in audits and quality assurance programs to monitor the effectiveness of transplant services and drive improvements. Engage in ongoing professional development to stay updated on best practices in transplantation and regulatory changes affecting transplant care.
9. Education and Training of Staff:
Organise and participate in local/national/international conferences to share the knowledge and learnings. Serve as a resource and provide training to other healthcare professionals, including nursing/medical/surgical staff and allied health professionals, on the transplant process and patient care. Conduct educational sessions, workshops/seminars within the NHS trust to enhance the transplant team’s knowledge and skills. Assist in the orientation of new transplant team members and contribute to developing educational materials to support transplant services.
10. Research and Contribution to Transplant Advancements
Support and participate in research initiatives, helping collect data and contribute to studies aimed at improving transplant outcomes. Collaborate with research teams on transplant-related studies, clinical trials, and quality improvement projects. Engage with professional networks and transplant associations to promote best practices, share insights, and foster advancements in transplant care.
Conclusion:
The LTPC is crucial in ensuring the continuity, quality, and safety of transplant patient care, providing a compassionate approach and high-level clinical expertise within the field. LTPC remains the point of contact for patient/family from and the local health care provider from their initial stage of transplant journey until the end. The role is incredibly fulfilling and requires excellent interpersonal and organisational skills.
This article is based on the authors' experiences at King's College Hospital, highlighting the unique approaches and job descriptions for LTPC that may differ across various centers. It's important to consider these variations when exploring the topic.
*For further information on the role of the liver transplant coordinator please refer to The Royal College of Nursing. (n.d.). Caring for people with liver disease | Publications | Royal College of Nursing. [online] Available at: https://www.rcn.org.uk/professional-development/publications/pub-007733. This framework describes the professional standards expected of practitioners when caring for people with liver disease including liver transplantation. It includes competencies for liver transplantation. This publication is currently being reviewed; an update is planned for 2025.*
3 identified learning points.
1. Key role of Liver Transplant Coordinator.
2. Patient Advocacy service- Long term and sustainable professional relationship with patient and family
3. LTPC’s are an integral part of Transplant unit and perform autonomous role
A list up to 5 key words
Organ
Liver
transplant
coordinator
Roles
References:
- Pradeep A, Barker F, Ramos K, Littlejohn W, Tavabie D O, Nicholson C, Menon K, Cramp M, McDougall N, Cash J, Aluvihare V (2021) Virtual liver transplant assessment a novel pathway that is likely safe, effective and optimise access to transplantation. Frontline Gastroenterology Journal
Author Biographies
 Dr. Agimol Pradeep BEM, Senior Transplant Coordinator at Kings College Hospital, London.
Dr. Agimol Pradeep BEM, Senior Transplant Coordinator at Kings College Hospital, London.
She completed her nursing studies in India and has been working in NHS care settings since 2001. She is also a philanthropist to promote Black and Asian Minority Ethnic (BAME) organ and stem cell donation awareness. Her PhD on the topic of “Increasing organ donation in the North West South Asian community through targeted education” impacted positively on this sensitive topic by understanding South Asians' attitudes and their health behaviours and beliefs and implementing targeted education to change their beliefs and attitudes towards organ donation. She has been working closely with NHSBT in her volunteer capacity since 2010 and remains a steering group member for the Community Investment Scheme. Her contribution to the community in promoting the organ donation message was recognised nationally, and she received the British Empire Medal (BEM) in 2018 and Nurse of the Year in 2015 from the British Journal of Nursing. She initiated the campaign in 2020 to support Internationally Educated Nurses (IEN’s) working in the UK as unregistered practitioners. Played a key role in reviewing the NMC's English language requirement policy and implementing the Supporting Information from Employer (SIFE) pathway, to enable the IEN’s to complete their UK registration. She remain as the NMC’s Expert Advisory Group member of the English Language Review Group. This initiative was recognised by the Health Service Journal (HSJ) for workforce initiative in 2023. She is a member of the Royal College of Nursing's (RCN) international committee. She also serves as a reviewer for nursing and transplant journals.

Sarah Coate, Lead Liver Transplant Co-ordinator at Kings College Hospital, London.
I have worked in liver transplant since 2004, firstly on the Liver intensive care unit. I then became a transplant coordinator in 2008 and have loved the role. My interests are post-transplant pregnancy and long-term care of the transplant recipient. More recently I have taken on a leadership role in the liver unit and now manage the transplant coordinator team.
Karen Mercer, Nurse Advisor, British Liver Trust.
I graduated from Kings College London in 1995 and commenced work on the liver wards at Kings College Hospital. Having received 1 liver lecture during my training, I was fascinated to see the breadth and depth of issues facing patients with liver disease and have remained within the field for 30 years. During my 30 years I have worked across a variety of liver focussed services, and have set up 2 viral hepatitis services in NHS Hospitals. I returned to the liver transplant service at Kings where I was 1 of 2 nurse specialists who established a post-transplant nurse led clinic which proved vital during the pandemic and led the transplant coordinator team until January 2025. I have recently joined the nurse advisor team at The British Liver Trust. Transitioning from the NHS to the charity sector is a work in progress, but I am embracing the opportunity to encounter patients outside of hospital services who are affected by liver issues.

Krizyl Anne dela Cruz Alés, Liver Recipient Transplant & Live Liver Donor Coordinator at Kings College Hospital, London.
Graduate Bachelor of Science in Nursing at Silliman University, Dumaguete City, Philippines in 2009. After passing the Philippine Licensure Exam, she worked as an ICU nurse at Holy Child Hospital, Dumaguete City and stayed there for over 4 years. She then had a short stint at Mount Elizabeth Novena Hospital, Singapore as an ICU nurse. She subsequently moved to the UK in November 2017 and worked as a staff nurse at King's College Hospital Liver Intensive Therapy Unit before progressing in her career as a band 6 in Critical Care Unit B at the same hospital. She joined the Liver TPC team in November 2022.
 Tiffany Recato Dy, Liver Recipient Transplant Coordinator, at Kings College Hospital, London.
Tiffany Recato Dy, Liver Recipient Transplant Coordinator, at Kings College Hospital, London.
I have received my qualifications in the Philippines in 2010. I have worked in a general ICU back in the Philippines, for 3 years. I have moved to Liver Intensive Care unit at Kings and got exposed to the wonders of liver transplantation. After 5 years of working in Liver Intensive Care Unit, I felt that I still dont have enough knowledge on liver transplantation and wanted to explore this role. I applied and became one of the liver recipient transplant coordinator in 2019. Since then, I have never looked back, enjoyed working and learning about transplantation.
Miranda Coles, Liver and Pancreatic Islets Recipient Transplant Coordinator.
I qualified as an Adult Nurse in 2011 at Bournemouth University and my first ever job was at King's College Hospital in London spending 18 months on an Acute Medical Rotation. In 2013, I chose a daring journey and begun my career specialising in liver diseases by nursing in the Kings' Liver Intensive Care Unit. I spent 5 years here, progressing to Junior Sister in my 4th year. I was exposed to, and became interested in, Liver Transplantation very early on in my Intensive Care career, often asking if I could nurse the patients immediately post-transplant or the patients in Acute Liver Failure awaiting their emergency lifesaving transplant. In September 2017, I officially became a Liver Transplant Coordinator have been in this position for 8 years! I have also taken on extra roles, such as the King's Pancreatic Islet Transplant Lead Coordinator and have never looked back!