An introduction to endoscopic vacuum therapy for Upper Gastrointestinal defects
Authors: Nasar Aslam, Yassar Qureshi, Vinay Sehgal
Contributors: David Leonard, Rawen Kader, Sally Thorpe, Omer Ahmad, Matthew Banks, David Graham, Khaled Dawas, Borzoueh Mohammadi, Rami Sweis - University College London Hospitals
Introduction
Vacuum assisted closure (VAC) of external wounds is a well-established surgical technique used for the management of external surgical wounds. (1) Negative pressure suction applied through a specialised dressing leads to drainage of excess fluid, reduces associated oedema and promotes the formation of granulation tissue. Furthermore, the negative pressure encourages the defect edges to come closer together. This multifactorial process leads to accelerated tissue healing through secondary intention measures.(2)
Endoscopic vacuum therapy (EVT) exploits these same mechanistic properties to enable the minimally invasive treatment of gastrointestinal defects. Although EVT is a novel and emergent area of GI endoscopy it is proving to be a very successful treatment option. (3)
Historically the management of upper gastrointestinal (GI) defects remained primarily surgical with those not fit enough for surgical intervention being managed conservatively with antibiotics and total parenteral nutrition. Consequently, this patient group was associated with a high mortality and morbidity rate. (4)
The introduction of endoscopic treatment in recent years is starting to cause a paradigm shift in how this patient cohort is managed and thus leading to more favourable outcomes.
Outline
In this web education article, we aim to cover the following aspects of EVT.
- Overview of Gastrointestinal defects
- How does vacuum therapy work
- How to perform EVT
- Advantages of EVT
- Disadvantages of EVT
- When not to use EVT
1. Overview of Gastrointestinal defects
Transmural upper GI defects are defined by full thickness rupture of the GI wall. Broadly speaking they can be subcategorised into leaks, fistulas, and perforations. These defects are summarised in table one below.
Type of defect | Definition | Cause |
Perforation | Acute rupture of GI wall | Iatrogenic: Post surgical, Endoscopic
Spontaneous: Boerhaaves |
Leak | Defect leading to pathological communication between intra and extra luminal space | Post-surgical |
Fistula | Connection between two epithelised surfaces | Chronic inflammation Malignancy Untreated leak |
Table 1: Overview of leaks, fistulas and perforations.
Endoscopic closure with clips, sutures, stents and tissue sealants can be considered however in cases with an associated cavity or those where primary closure with conventional treatment has failed an unmet need exists and EVT has started to play a role in fulfilling this unmet need.
EVT offers several synergistic benefits which work in tandem to accelerate wound healing and defect closure. Negative pressure suction helps to clear secretions and exudate from the defect. This keeps the defect dry allowing an optimal environment for granulation tissue formation at the defect edges. Furthermore, it also leads to enhanced microcirculation at the defect edges which optimises the conditions for wound healing. (2)
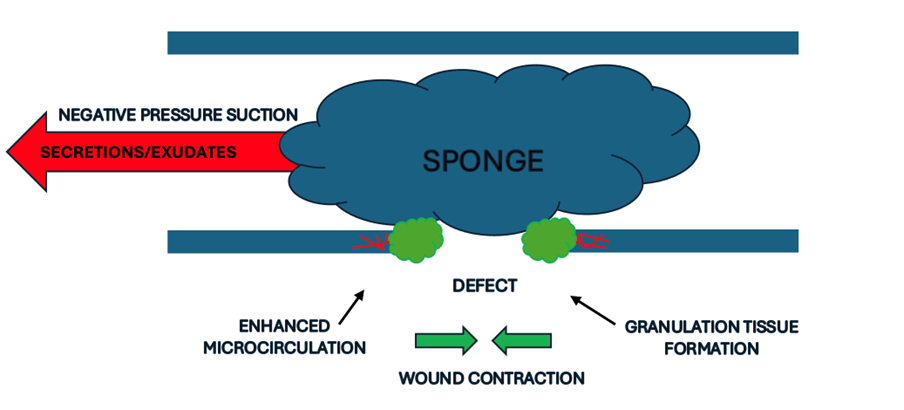 Figure 1: Underlying physiological changes associated with EVT
Figure 1: Underlying physiological changes associated with EVT
3. How to perform endoscopic vacuum therapy?
EVT can be performed either intracavitary or intraluminal. We would recommend any endoscopic intervention on patients with luminal defects be performed using carbon dioxide insufflation due to its rapid absorption. Typically, patients with a sizeable cavity associated with a luminal defect will require a period of intracavitary sponge therapy to reduce the size of the cavity. Although it’s possible to self-fashion devices for EVT there are proprietary devices that have been specially designed for this purpose. Intracavitary sponge therapy can be performed with an EsoSpongeTM (Figure 2). This is a device which has a sponge and associated suction catheter. Placement typically involves inserting an over tube adjacent to the defect and then guiding the sponge through the over tube and into the defect using grasping forceps. Prior to insertion it is imperative to soak the sponge in water to limit the amount of friction during insertion. Exchange is performed every 72 hours where the sponge size is reduced in accordance with reduction in the cavity size. Sponge exchange is necessary at frequent intervals to reduce the risk of sponge embedment which can make removal difficulty and increase the risk of GI haemorrhage.

Figure 2: EsoSpongeTM (Boston Scientific)
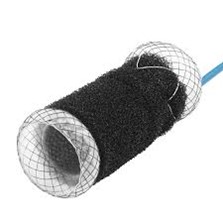 Figure 3: VacStent GITM(Micro-tech)
Figure 3: VacStent GITM(Micro-tech)
Intraluminal sponge therapy can also be performed with the EsoSponge however for oesophageal defects there is a novel device called the VacStent (Figure 3) which combines the benefits of both stent and vacuum therapy. This device is exchanged every 7-10 days until defect closure is achieved. Literature supports a median of 2.5 exchanges being required for definitive closure.
Both the EsoSponge and VacStent are connected to a negative pressure wound pump (3M V.A.C Ulta, Figure 4) via suction catheters. The typical starting pressure for the VACstent is -125mmHg for the VacStent and similar for the EsoSponge however some locoregional variation in practice exists across Europe.

Figure 4: 3M V.A.C Ulta
4. Advantages of Endoscopic Vacuum Therapy
- Enhanced Recovery -The conventional standard of care for patients with anastomotic leaks and transmural defects is associated with prolonged hospital stays whereas EVT exploits physiological processes to accelerate wound healing and defect closure. (5)
- High success rates for anastomotic leaks - Reoperation for anastomotic leaks is associated with considerable mortality and low success rates. EVT however has demonstrated clinical success rates of roughly 70% for patients with anastomotic leaks.(5)(6)(7)
- Minimally invasive - EVT does not require surgical intervention and is performed endoscopically which results in less post procedural discomfort for the patient and a less traumatic post procedural journey for the patient.
- Versatility - As the defect associated cavity reduces in size the sponge can be resized accordingly, and treatment can be adapted from intracavitary to intraluminal once the cavity is no longer sizeable for sponge therapy.
- Sepsis control - EVT draws secretion and exudates away from the defect which helps to decrease bacterial contamination and consequent septic episodes.
- Liberation from parenteral nutrition (VACstent) - As the VacStent is a fully covered stent and its placement is secure due to the negative pressure component applied to the sponge the risk of slippage is mitigated. Consequently, patients can resume oral intake and be liberated from nil by mouth status and parenteral nutrition. It is important to note that this however does not apply to EVT with the EsoSponge as this does not seal the defect.
5. Disadvantages of Endoscopic Vacuum Therapy
- Frequent endoscopic intervention and operational considerations - Both intracavitary and intraluminal EVT requires frequent exchanges. The Esosponge requires exchange every 48-72hours and the VacStent requires exchanging every 7-10 days. This is to reduce the risk of the sponge getting embedded and facilitate easier removal/exchange. This ultimately requires trained endoscopists at hand to facilitate EVT according to the treatment pathway.
- Specialist equipment and required skill set - EVT is a technically challenging procedure and as such requires appropriately trained and skilled operators to facilitate insertion and exchange. Furthermore, the device requires considered set up and removal in addition to nursing staff who can manage a negative pressure wound pump.
- Potential for serious adverse device effects (SADE) - There is an inherent risk with EVT which includes extension of the defect, GI haemorrhage and sponge embedment all of which need to be considered, and patients be consented for.
- Short term cost considerations - Both the EsoSponge and the VacStent come with upfront costs associated with the device, need for frequent endoscopic interventions and individual negative pressure wound pumps. However, over the longer term they do result in a significant reduction in length of stay which can offset the associated short term financial implications.
- Limited use in fistulas with airway involvement - In cases of aerodigestive fistulas vacuum therapy may be precarious as the negative pressure suction can lead to airway compromise. Although there is no clear guidance in this space and a few case reports have demonstrated the efficacy of vacuum therapy in this area. It is generally considered a relative contradiction for EVT. (8)
6. When not to use endoscopic vacuum therapy
As EVT is a novel treatment option with no randomised controlled data to support its use limited consensus exists on when EVT should be adopted over alternative endoscopic closure methods. However, it is prudent that patients being considered for EVT should have multidisciplinary team discussion with close surgical and gastroenterological collaboration. Although wide ranging indications for EVT exist there are certain scenarios where it should be avoided.
EVT should not be used in the following scenarios:
- Chronic defects where tissue viability is compromised
- Large aerodigestive fistula’s
- Overwhelming sepsis and contamination
- Patient tolerance concerns
- Endoscopically inaccessible defects
Conclusions
EVT is playing an increasingly pivotal role in the treatment paradigm for the management of gastrointestinal transmural defects. As experience expands and the evidence base grows, we will be able to identify appropriate cases based on defect phenotype and the pre-test probability of treatment success. At present the cornerstone of successful management is close surgical and GI collaboration.
References
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563–76; discussion 577.
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563–76; discussion 577.
- Binda C, Jung CFM, Fabbri S, Giuffrida P, Sbrancia M, Coluccio C, et al. Endoscopic Management of Postoperative Esophageal and Upper GI Defects—A Narrative Review. Medicina. 2023 Jan;59(1):136.
- Turrentine FE, Denlinger CE, Simpson VB, Garwood RA, Guerlain S, Agrawal A, et al. Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg. 2015 Feb;220(2):195–206.
- Möschler O, Nies C, Mueller MK. Endoscopic vacuum therapy for esophageal perforations and leakages. Endosc Int Open. 2015 Dec;3(6):E554–8.
- 770. CLOSURE OF OESOPHAGEAL DEFECTS USING THE VACSTENT DEVICE: INITIAL INSIGHTS FROM THE LARGEST UK CASE SERIES | Diseases of the Esophagus | Oxford Academic [Internet]. [cited 2025 Apr 19]. Available from: https://academic.oup.com/dote/article/37/Supplement_1/doae057.371/7747088
- Lange J, Kähler G, Bernhardt J, Knievel J, Dormann A, Hügle U, et al. The VACStent trial: combined treatment of esophageal leaks by covered stent and endoscopic vacuum therapy. Surg Endosc. 2023 May;37(5):3657–68.
- Kamaleddine I, Popova M, Alwali A, Schafmayer C. Endoscopic Vacuum Therapy for Treating an Esophago-Pulmonary Fistula after Esophagectomy: A Case Report and Review of the Literature. Visceral Medicine. 2023 Apr 12;39(1):18–24.
Author Biographies

Dr Nassar Aslam
Dr Nasar Aslam is a Consultant Gastroenterologist with a sub-specialist interest in upper gastrointestinal disorders and advanced therapeutic foregut endoscopy. His interests includes endoscopic vacuum therapy (EVT), cryoablation, and the management of complex oesophageal and gastroduodenal pathology. He has contributed to outcome evaluation for the largest UK series using the VACStent, presenting findings at national and international meetings, and is actively involved in assessing outcomes for cryoablation therapy in Barrett’s Oesophagus. Dr Aslam initially developed his expertise in oesophageal disease through a dedicated fellowship under Dr Rehan Haidry and Professor Laurence Lovat at University College London, before undertaking an interventional endoscopy fellowship at UCLH under the supervision of Dr Vinay Sehgal. During this time, he was awarded the national BSG Out-of-Programme Trainees Award to support of his academic and clinical contributions. He plays an active role in both national and international professional societies. Dr Aslam serves as the UK representative to the United European Gastroenterology (UEG) Meeting of Members and is a member of the Education Committee of the International Society for Diseases of the Esophagus (ISDE). He was recently elected to the British Society of Gastroenterology (BSG) Endoscopy Clinical Research Group and the BSG Gastroduodenal Section. In addition to his clinical and research interests, Dr Aslam is dedicated to medical education and service innovation, regularly contributing to trainee mentorship, academic development, and the adoption of novel endoscopic technologies in clinical practice.
 Mr Yassar Qureshi
Mr Yassar Qureshi
Mr Yassar Qureshi is a Consultant Surgical Oncologist at University College London Hospital, with a focus on surgery for oesophago-gastric malignancy. In addition to his cancer interest, he also provides a benign oesophageal disease service, for high-risk and complex cases, including surgery for emergency oesophageal perforations. Within this context, he is involved in a major study assessing Endoscopic Vacuum Therapy (EVT) to investigate its safety and effectiveness in defect closure. Yassar maintains an active interest in research and development in his field, having authored several book chapters and over 20 peer-reviewed manuscripts. His doctorate studied the impact of complications on Upper GI cancer survivorship, and novel methods to monitor, treat and reduce these. He maintains a leading interest in several ongoing studies to enhance peri-operative optimisation for Upper GI cancer patients. He regularly works as a humanitarian surgeon and has developed a personal interest in establishing a global collaborative to improve training and surgical advancement in less developed countries.

Dr Vinay Sehgal
Dr Vinay Sehgal is a Consultant Gastroenterologist, Interventional Endoscopist and Associate Professor at University College London Hospital (UCLH). His clinical interests focus on the early detection of pre-malignant lesions of the upper gastrointestinal tract including Barrett’s Oesophagus and Oesophageal Squamous Cell Neoplasia. He has a particular expertise in endoscopic technologies including advanced imaging, resection and endoscopic defect closure using various endoscopic suturing platforms. He also had a specialist interest in ‘third space’ endoscopy and routinely performs procedures such as per-oral endoscopic myotomy (POEM), Zenker’s-POEM and endoscopic submucosal dissection (ESD) in his clinical practice. He is the Principal Investigator (PI) for the European C2 Cryoballoon Ablation Registry who is collecting important real-world outcomes on Cryoballoon Ablation for the treatment of Barrett’s Oesophagus. He is also the UK PI for Endoscopic Vacuum Therapy (EVT) to investigate this technologies safety and effectiveness in defect closure and post-operative leaks. Dr Sehgal has a keen interest in training and is the Endoscopy Training Lead at UCLH. During this time, he was awarded the prestigious British Society of Gastroenterology (BSG) Dame Parveen Kumar Award for Education and Training in June 2025. Due to commitment to endoscopy, training and research, he has recently been successfully elected as a member of the Endoscopy Committee at the BSG.