Introduction
Symptoms of anorectal dysfunction, which are characterised by faecal incontinence (FI) and/or constipation/an evacuation disorder (ED), cause significant morbidity and can have devastating effects on patient’s quality of life. As the underlying aetiology and pathophysiology of both FI and ED’s is often multifactorial, reliance on symptoms alone is inadequate as the sole means of directing therapy [1,2]. Thus, when initial management strategies fail, anorectal function testing is a key component of the clinical evaluation [2]. Although there is no set gold-standard test of anorectal function, anorectal manometry is the best-established investigative tool to objectively assess sensorimotor function [1,2,3]. Recently, the International Anorectal Physiology Working Group published recommendations for a standardised anorectal manometry protocol and a new classification system (the London Classification) to describe the results of diagnostic testing in patients with disorders of anorectal function [4]. This narrative review aims to assess the usefulness of the protocol and London classification to investigate and diagnose non-malignant disorders of anorectal function using high-resolution anorectal manometry (HR-ARM).
Clinical Indications
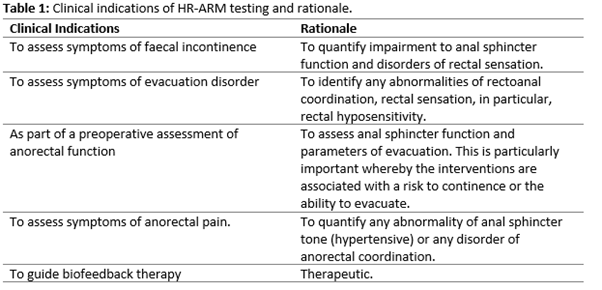
Manometric assessment should be reserved for patients in whom serious underlying pathology (such as colorectal malignancy and inflammatory bowel disease) has been appropriately excluded (e.g. at colonoscopy), and symptoms remain refractory to standard conservative or medical therapies. The choice of investigations requested is guided by the clinical history, examination, and local resources. At a minimum, anorectal manometry including evaluation of rectal sensation should be undertaken to assess anorectal sensorimotor function and be accompanied by a direct assessment of evacuation (e.g. defecography or the balloon expulsion test [BET]) in those patients with symptoms of an evacuation disorder [2, 4]. However, no single test can fully assess anorectal function, and other complementary investigations should be considered (e.g. endoanal ultrasound for assessing anal sphincter structure, whole-gut transit studies etc.) as indicated [2,3]. The principal indications for HR-ARM are outlined in Table 1 below.
The International Anorectal Physiology Working Group (IAPWG) Protocol
To standardise the clinical measurement and nomenclature of anorectal function, the International Anorectal Physiology Working Group (IAPWG) developed an internationally recognised consensus-based protocol [4]. Whilst not fully diagnostic, the IAPWG recommends the performance of a digital rectal examination (DRE) prior to anorectal manometric intubation to provide an indication of anorectal and pelvic floor anatomy and function and should also exclude faecal loading. A DRE may also be utilised to check patients understanding of specific test manoeuvres such as “squeeze” and “push”.
The IAPWG protocol consists of the following sequential elements [4]:
- 3 minute stabilisation period – performed to allow pressures in the anal canal to return to baseline following intubation.
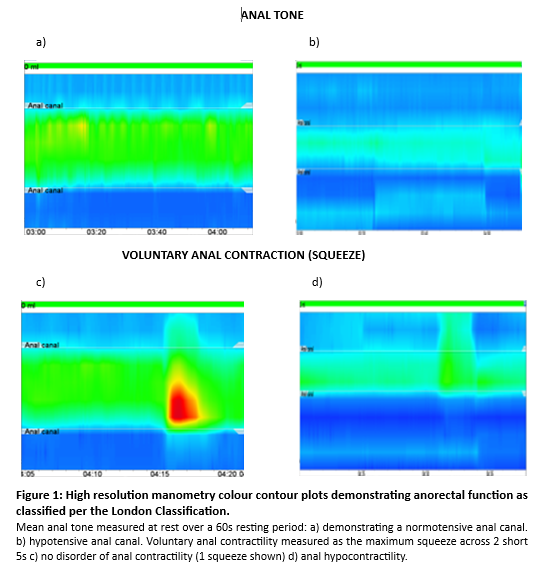
- Resting pressure – a measurement of anal tone at rest recorded across a 60s period. The mean resting pressure is quantified and recorded. Ultra-slow waves may be observed and should be reported.
- Voluntary squeeze (short) – the patient should be asked to squeeze for 5s, and this should be repeated 3 times with each attempt separated by a 30s recovery period. The most qualitatively normal squeeze should be quantified with maximum incremental pressure reported (Figure 1c & 1d).
- Endurance squeeze – a single endurance squeeze is the measure required to assess both the contractility and fatigability of the striated external anal sphincter muscle across 30s. This should be followed by a 60s recovery period.
- Cough – two single coughs are performed each separated by a 30s recovery period. A quantitative measure of the maximum pressure changes in both rectal and anal pressures should be reported. This is to demonstrate the normal protective reflex (anal pressure exceeding rectal pressure) during cough which causes an increase in intra-abdominal / intra rectal pressure.
- Push - measures recto-anal coordination during simulated defecation. Three pushes each of 15s duration are performed with each push separated by a 15s recovery period. The most qualitatively normal push should be used for analysis
- Rectal sensory testing – measures rectal sensitivity in response to rectal distention utilising a balloon attached to the catheter tip. Ramp or phasic distension may be used. For ramp distension, a rate of 2 mL/s is recommended and for phasic distension the inflation rate should be set to 10 mL/s. A quantitative measurement of ballon volume should be recorded for each of the patient reported sensory thresholds: first constant sensation volume, desire to defecate and maximum tolerated volume.
- Recto-anal inhibitory reflex (RAIR) – measures the reflex reduction in maximum anal canal pressures in response to rapid rectal distension. A starting volume of at least 30 mls should be used but a failure to elicit a RAIR may be seen with low distending volumes in a large capacity rectum. Thus, if a megarectum is suspected, the test should be repeated with increasing balloon volumes up to a maximum of 360 mls (or maximum toleration).
- BET or defecography – the results of a HR-ARM study should be considered in conjunction with a direct test of evacuation. The BET assesses an individual’s ability to expel a 50ml water-filled balloon whilst in a seated position. Defaecography assesses a patient’s ability to expel neostool (contrast) whilst either seated (fluoroscopic imaging) or in a left lateral position (magnetic resonance imaging).
Utilising the IAPWG protocol, the measurements, as described above, are necessary to complete each of four algorithms embedded within the London Classification. Each of the four parts and their resultant diagnoses are outlined in the Table 2 below [4].
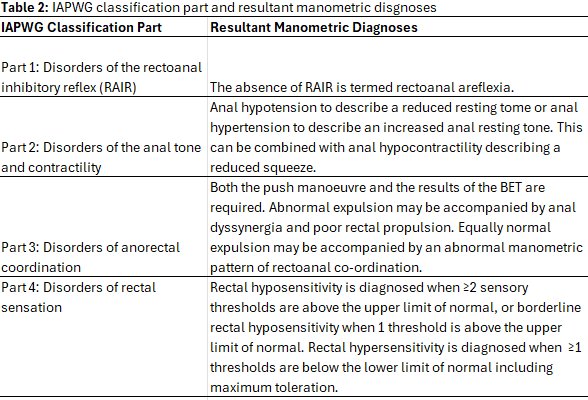
For each part of the classification, the clinical relevance of each manometric diagnoses is indicated via a hierarchical division of findings into: ‘major’, ‘minor’ and ‘of questionable’ clinical significance.
Discussion
Overall, the valuable efforts of the IAPWG in developing the London classification has been a first major step in generating a consensus agreement and set minimum standards for the performance and analysis of HR-ARM. A standardised protocol was required to reduce the number of discrepant methods of data acquisition, analysis, and interpretation; factors which hinder data generalisability and makes the comparison of data between centres and the pooling of data for large multicentre studies difficult [5].
Due to such historical variability in clinical practise, a paucity of data is available to support each protocol / classification element, and thus it must be noted that both are primarily based on a coalescence of expert opinion, rather than to a systematic review of clinical evidence. Since publication of the consensus document, however, the evidence-base is growing. By way of example, Ang et al, have shown that a 30s resting period provides equivalent diagnostic accuracy as a 60s resting period (as per the IAPWG recommendations) [6]. Nevertheless, the recommendations should be considered as a proposed standardised approach rather than a validated scientific methodology. As such, the healthcare professional should note that an ‘accepted’ abnormal finding may not constitute dysfunction. For example, Grossi et al., identified features of dyssynergia in 87% of healthy volunteers [7].
Furthermore, the test manoeuvres incorporated in the IAPWG protocol have been derived from ‘conventional’ manometry studies and may not best evaluate all aspects of anorectal function (2). For example, a refinement of physiological parameters such as the generation of a ‘contractile integral’ has been shown to improve sensitivity for detecting anal hypocontractility in FI from 32% to 55% when compared with the maximum squeeze increment [8]. Other technological advancements have led to the development of 3D ‘high definition’ ARM, incorporating 256 pressure sensors, which benefits from its ability to define functional anatomy of the anal canal [9].
Conclusions and learning points
- Overall, the IAPWG protocol and the London Classification provides an internationally recognised standardised protocol and nomenclature for the assessment of anorectal sensorimotor function. The adoption of these is necessary to bring about much needed harmonisation to clinical practice.
- However, it should be noted that no single test can be expected to fully characterise anorectal function and thus the results of HR-ARM should be complemented by the results other investigations.
- Nevertheless, the IAPWG protocol and London classification provides a standardised benchmark from which others in the field can judiciously appraise their performance through high quality clinical research. This will enable the development of future iterations, which should further improve diagnosis and management of patients with disorders of anorectal function.
Please see the References for this article below the CME information.
Author Biographies

Niamh Kavanagh, Clinical Scientist, Pelvic Floor Unit, Guy’s and St Thomas’ Hospital
Niamh Kavanagh qualified as a Clinical Scientist in 2023. After studying Biology at the University of Leeds, she completed the Scientist Training Programme at the Northern Care Alliance NHS Foundation Trust, specialising in gastrointestinal physiology and urodynamic science. She now works in the Pelvic Floor Unit at Guy’s and St Thomas’, providing specialist diagnostic testing for pelvic floor dysfunction and contributing to wider service delivery.

Elisa Skinner, Consultant Clinical Scientist, Northern Care Alliance
Elisa started her career in GI Physiology in 1998 at The Middlesex Hospital (now UCLH), followed by a short interval at St Mark’s Hospital. Elisa moved to Salford Royal Hospital in 2005 where she has been steering the GI Physiology service since 2008. Elisa has been involved with AGIP committee since 2004 periodically with the role of education secretary on several occasions.
CME
BSG Future Workforce Report
18 September 2024
- Scott SM, Gladman MA. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterology clinics of North America. 2008 Sep 1;37(3):511-38.
- Carrington, E.V., Scott, S.M., Bharucha, A., Mion, F., Remes-Troche, J.M., Malcolm, A., Heinrich, H., Fox, M., Rao, S.S. on behalf of the International Anorectal Physiology Working Group and the International Working Group for Disorders of Gastrointestinal Motility and Function. Advances in the evaluation of anorectal function. Nature Reviews Gastroenterology & Hepatology. 2018 15(5), pp.309-323.
- Scott SM, Carrington EV. The London classification: improving characterization and classification of anorectal function with anorectal manometry. Current Gastroenterology Reports. 2020 Nov; 22:1-2.
- Carrington EV., Heinrich H, Knowles CH., Fox M, Rao S, Altomare DF., Bharucha AE., Burgell R, Chey ED., Chiarioni G, Dinning P, Emmanuel A, Farouk R, Felt-Bersma RJF., Jung KW., Lembo A, Malcom A, Mittal RK., Mion F, Myung SJ., O’Connell PR., Pehl C., Remes-Troche JM., Reville RM., Vaizey CJ., Vitton V., Whitehead WE., Wong RK., Scott SM. All members of the International Anorectal Physiology Working Group. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterology and Motility. 2020. 32(1), e13679.
- Bellini M, Chiarioni G. Staying in HR-ARM’s way: tweaking the London Classification for disorders of anorectal function. Digestive Diseases and Sciences. 2022 Mar;67(3):748-9.
- Ang D, Vollebregt P, Carrington EV., Knowles CH., Scott SM. Redundancy in the International Anorectal Physiology Working Group Manometry protocol: a diagnostic accuracy study in fecal incontinence. Dig Dis Sci. 2022 Mar;67(3):964-970.
- Grossi U, Carrington EV, Bharucha AE, Horrocks EJ, Scott SM, Knowles CH. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut. 2016 Mar 1;65(3):447-55.
- Carrington EV., Knowles CH., Grossi U., Scott SM. High-resolution anorectal manometry measures are more accurate than conventional measures in detecting anal hypocontractility in women with faecal incontinence. Clinical Gastroenterology and Hepatology. 2019. 17:477-485.
- Zifan A, Ledgerwood-Lee M, Mittal RK. A predictive model to identify patients with faecal incontinence based on high-definition anorectal manometry. Clinical Gastroenterology and Hepatology. 2016. 14 (12): 1788-1796.
