Shingles vaccine (Shingrix) now recommended for all severely immunocompromised adults aged 18 and over
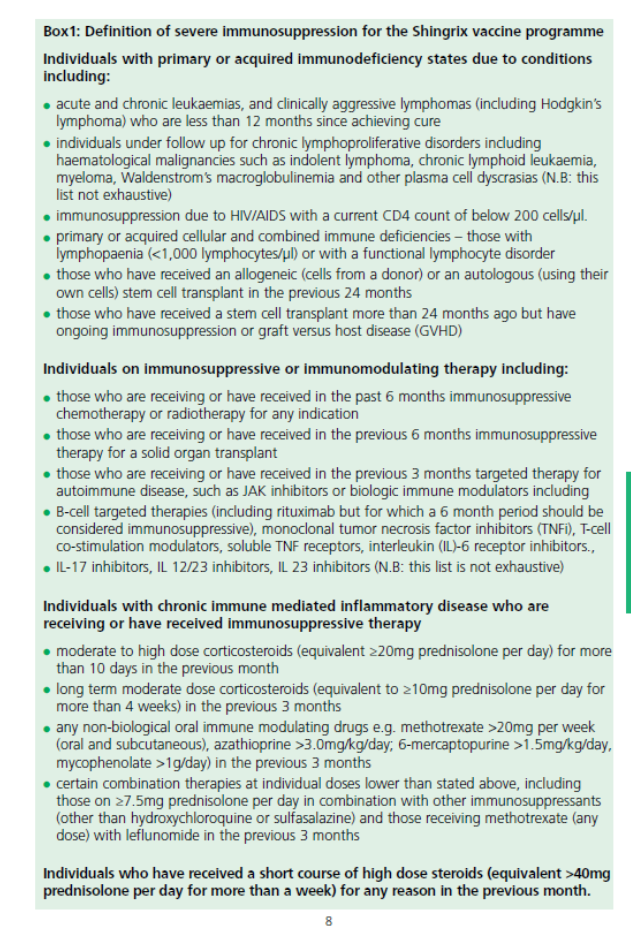
Full details of the policy are shown in the Green Book which includes a national implementation plan, ensuring equitable access to vaccination for all eligible immunosuppressed adults, including those with IBD and chronic liver disease.
For maximal efficacy, two doses of RZV are necessary regardless of previous history of shingles or receipt of zoster vaccine live (ZVL, Zostavax). The second dose is recommended 2-6 months after the first. Where possible, patients should be vaccinated before becoming immunosuppressed, and the second dose can be administered 1-2 months after the first if needed. In practice this should mean that adult patients starting or established on advanced therapies and /or on oral prednisolone doses of (preferable at doses of <20mg for improved effectiveness), can benefit from Shingrix vaccination.
In England, Wales and Northern Ireland, GPs have been commissioned to deliver the vaccination in primary care so please consider adding text recommending the vaccination (and other vaccines) to your clinic letters to remind colleagues in primary care.
In Scotland, vaccinations are not provided by GPs. Please review the information on central vaccination centres.
Thanks go to Dr Shahida Din and the BSG IBD Section committee who have played a key role in advocating for this change through research and policy work.