BSG CSSC Service Development Prize 2023 highly commended submission by Dr Mark McAlindon
Names of team involved: McAlindon ME, Shivakumar V, Neill G, McKenzie S, Oka P, Sidhu R, Turvill J.
Challenges and the need to change
The suspension of routine endoscopy during the COVID pandemic stimulated a rethink to accepted practice: that conventional endoscopy, performed in 1-2% per annum, invasive, uncomfortable, resource intensive, associated with risks of intubation and sedation, is the first line diagnostic tool despite rarely identifying malignancy. [1] Alternatives are needed to mitigate pressures on endoscopy services and provide safer, more accessible, patient acceptable primary diagnostic tools.
Overcoming the challenges
In anticipation of post-pandemic service pressures, the BSG Endoscopy COVID Research Group addressed the role of novel technologies in 2020. [2] Capsule endoscopy is rapidly evolving: dual camera devices with high frame capture rates provide comprehensive imaging of oesophagus, colon and small bowel and magnetic control allows gastric examination. It is non-invasive and preferred by patients. [1]
Oesophageal capsule endoscopy for varices surveillance
The PillCam ESO2 (Medtronic Ltd; 18 frames per second (fps)), has 85% sensitivity in oesophageal varices detection. [3] We described a novel nurse-led examination protocol using the UGI capsule (35fps; Medtronic) [4] and performed an observational cohort study of patients whose gastroscopies were suspended during the pandemic. The Endoscopy Concern Scale (ECS) was used to assess acceptability and a visual analogue scale to assess overall experience. [5]
Colon capsule endoscopy: national rollout
In response to the pandemic, NHS England provided £6m to Cancer Alliances to develop 2 week wait Colon Capsule Clinics. [6] A funded amendment to the Fast Track study (IRAS 156515) allowed prospective study of blood, FIT and colonic investigations.
Video interpretation using artificial intelligence (AI)
In the first prospective, multicentre, blinded study, AI software was compared to experts in capsule video reading in routine clinical practice. [ArtIC:7]
Gastric capsule endoscopy: paving the way for the future
Steering of a capsule in a water-filled stomach can be achieved using two joysticks to control polarity and distance of an external magnet suspended above the patient (Navicam: Ankon Ltd), We established an international TARMAC (Teaching and Research in MAgnet-controlled Capsule endoscopy (MACE)) group. Training exercises using ex-vivo models were designed, learning curves studied and competency defined using Cusum analysis. A multicentre study of anaemic patients having gastroscopy, small bowel capsule and colonoscopy aims to establish Bleeding Location In The GI Tract (BLITGIT): the same capsule is used for MACE before small bowel examination. Diagnostic yield of MACE and gastroscopy is being compared.
Outcomes
UGI capsule endoscopy in variceal surveillance
Capsule endoscopy was performed in 207 patients (median (IQR) age 62 (±18), 53% male, follow up 24 months (±19)). Views of oesophagus, cardia and fundus were complete in 99%, 86.5% and 52.2% respectively. Oesophageal transit was 7 seconds (±10; ≈ 945 images). 58 (28%) had oesophageal (grade (G)1: 38; G2: 14, G3: 3) or gastric varices (G1: 3) detected (figure 1). Management changed in 25 patients (12.1%: 12 medications and 13 gastroscopy (capsule retrieval in one)). Two patients subsequently required emergency G2 variceal banding: in one, no varices were seen four years earlier; the other, G1 varices 12 months earlier. [data submitted: BSG 2023] Post-procedure ECS scores: 36(±28) and 11(±1; P<0.001); overall experience 100(4) and 75(±45; P<0.001) respectively. [8]
The NHSE colon capsule endoscopy pilot
Hospitals trusts (n=51) reported on 2288 colon capsules (mean age 60y; 55% female; figure 2), 1239 colonoscopy and 143 CT colonography patients. Colon capsule completion rate was 73.4% overall. Completion rates were over 85% in centres adopting the new prucalopride-containing bowel preparation regimen. Adverse events were reported in 0.7% (16 cases: one capsule retention).
Cancer, polyps or inflammatory bowel disease were identified in 47.1%, 41.8% and 25.4% by colon capsule, colonoscopy and CT colonography patients and polyps ≥10mm were seen in 13.4%, 10.1% and 10.5% respectively. When complete and of adequate quality, colon capsule identified 98.4% of the patients with polyps ≥10mm found at subsequent colonoscopy. Only 30.3% needed further endoscopy (67.9% for polyp resection) and 36.5% of these were for flexible sigmoidoscopy only. [submitted BSG]
The ArtIC study
The diagnostic yield of lesions in AI-assisted reading (73.7%, n=98/133) was superior (p=0.035) to standard reading (62.4%, n= 83/133) and 8.8 times faster (p<0.001). [submitted BSG]
BLITGIT study: comparing MACE and gastroscopy
Patients (n=92) had lesions (defined as possible or likely causes of anaemia) in the upper GI tract (27.1%), small bowel (48.9%) and colon (29.3%; P=0.003). MACE and gastroscopy findings were concordant in 37.8%, MACE alone identified lesions in 53.3% and gastroscopy alone in 8.9%. Yield favoured MACE over gastroscopy (P<0.001). [submitted BSG]
Developing a MACE training programme
Competency identifying numbered markers in a water-filled plastic stomach (figure 3) was reached more quickly by non-endoscopists than endoscopists (43.8 and 68.0 attempts), younger (<30 yrs) novices (43.8 and 68.0) and gamers compared to non-gamers (38.5 and 66.0). [9] Early experience suggests that MACE competency in patients can be achieved in an intensive, hands-on TARMAC training programme of one week. If successful, this compares with a two year training programme of 200 observed gastroscopies required by the Joint Advisory Group on Endoscopy Training.
Learning points
Capsule endoscopy is being recognised by national organisations as potential first line diagnostic tools and technology is advancing rapidly.
Oesophageal capsule endoscopy is feasible, safe, preferred by variceal surveillance patients and associated with favourable outcomes.
The NHSE pilot, the largest prospective, multicentre colon capsule study, shows a very high sensitivity for polyp detection and avoids conventional endoscopy in 70% of intermediate risk patients.
Capsule endoscopy AI software is more sensitive and much faster than human reading.
Gastric capsule using magnet control identifies more lesions and preliminary data suggests that novices can become competent very much quicker than in gastroscopy.
References
- Frontline Gastroenterol 2021;12:263-4.
- https://www.bsg.org.uk/medical-interest/endoscopy/
- Collie et al. Cochrane Database Syst Rev 2014(10):CD008760
- Ching et al. World Journal Gastroenterol 2018;24:2893-2901.
- Condon et al. Canadian Journal Gastroenterol 2008;22:41-47.
- https://www.england.nhs.uk/coronavirus/documents/covid-19-cancer-services-recovery-plan-14-december-2020/
- https://clinicaltrials.gov/ct2/show/NCT04821349
- McKenzie et al. Gut 2022;71:A128-A129.
- McKenzie S. B Med Sci 2022; University of Sheffield.
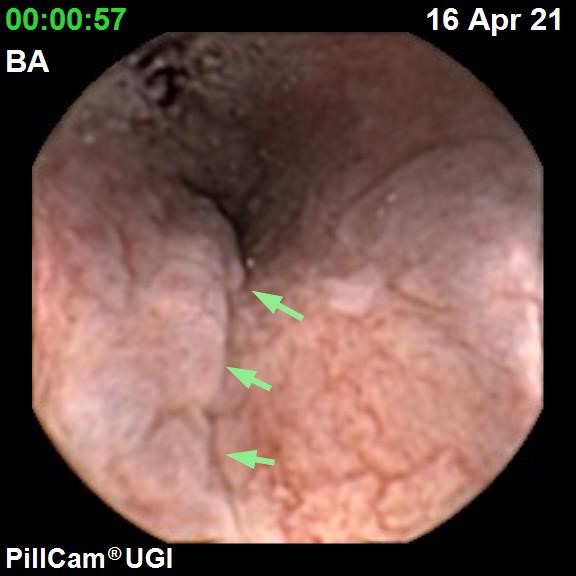
Figure 1. Small oesophageal varices seen using the UGI capsule

Figure 2. Colon capsule shown with data recorder and video being analysed on computer monitor
 Figure 3. Magnet-controlled capsule endoscopy system showing magnet robot, data recorder and belt, plastic stomach model and control station with joysticks and monitors.
Figure 3. Magnet-controlled capsule endoscopy system showing magnet robot, data recorder and belt, plastic stomach model and control station with joysticks and monitors.
Read More

