Author: Professor Ali S Taha MD PhD FRCP*, University Hospital Crosshouse & University of Glasgow, Kilmarnock KA2 0BE, Tel.: (44) 1563 827 280
Conflict of interest: None.
Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin, continue to be amongst the most commonly used drugs, both prescribed and bought over-the-counter; and they are likely to be used at this rate or even more for many years to come [1]. They have been recognised for their effective analgesic activities in the entire range of acute and chronic painful conditions [2]. Aspirin has also been used as an antiplatelet agent for the prevention of ischaemic vascular events [3]. Ideally, the use of these agents should be for as short a time as possible, and in as low a dose as possible.
However, in recent years, newer indications have been proposed for the long term use of these drugs, including the prevention of cancers [4,5]. Despite these benefits, the use of these agents has been associated with frequent gastrointestinal (GI) side effects [1,2]. This article discusses the nature of these side effects and their prevention and management.
Manifestations of NSAID GI Side Effects
NSAIDs can cause any GI symptoms including nausea, vomiting, heartburn, dysphagia, retrosternal or abdominal pains, and altered bowel habits. These can be explained by the damage they may cause to the oesophagus, stomach, duodenum, small, and large bowels [1,2,6]. This damage can be diagnosed by upper GI endoscopy, video capsule endoscopy or enteroscopy, and by colonoscopy. These procedures may reveal the presence of mucosal erythema, erosions, ulcers, punctate intra-mucosal haemorrhagic spots, or strictures. Active or fibrotic lesions affecting the pylorus or any part of the small bowel may present with obstructive symptoms. Intestinal or colonic lesions can sometimes be impossible to distinguish from inflammatory bowel disease, particularly Crohn’s. They may even raise faecal calprotectin level [7]. These manifestations highlight the critical importance of taking a careful history of the use of these drugs.
Despite these manifestations, NSAID related GI damage can be relatively asymptomatic or silent, presenting for the first time with one or more of the serious ulcer complications. These include upper GI bleeding (haematemesis or melaena); obscure (or small bowel) bleeding; or even colonic bleeding. They may also cause iron deficiency anaemia (typical of obscure bleeding); perforation; obstruction, as mentioned above; and sometimes death [1-3, 6-9].
Prevention and Management
You can’t beat them, don’t use them. In theory, this is the simplest way to prevent NSAID induced GI damage. In practice, this has not been possible in light of the benefits of these agents [1-5]. Attempts at using alternative analgesics have also been of limited success. This is because alternatives, such as opiate derivatives and gamma aminobutyric acid analogues (e.g., gabapentin), have no anti-inflammatory activity; and they cause side effects of their own, including drowsiness, nausea, vomiting, constipation, and the risk of addiction [10,11].
Use of milder NSAIDs. Individual NSAIDs differ significantly in their GI mucosal damaging potentials. Relatively mild preparations include ibuprofen, etodolac, meloxicam, and cyclo-oxygenase-2 enzyme selective inhibitors such as celecoxib and etoricoxib. These were found to be of equal anti-arthritic efficacy to naproxen and indomethacin but to cause fewer gastric and duodenal ulcers [12].
Eradication of Helicobacter pylori. Eradication of this infection has been useful in the prevention of gastric and duodenal ulcers while still using NSAIDs. However, this preventative effect does not last long [13]; NSAIDs can cause ulcers even in the absence of the infection; and the infection is irrelevant to mucosal damage found in the oesophagus, small or large bowel [1-3, 8, 9]. Moreover, the infection is becoming rare thanks to the use of cleaner water, general hygiene measures, frequent use of antibiotics, and the wide implementation of test-and-treat strategies used in the management of dyspepsia [14].
No acid, no ulcer. This dictum has proven its efficacy since it was first proposed by Schwartz more than 100 years ago [15]. Gastric acid secretion suppressants, particularly proton-pump inhibitors (PPIs) and the newly introduced potassium–competitive acid blockers (P-CABs), have been very successful in both the prevention and healing of NSAID-related ulcers and erosions affecting the oesophagus, stomach, or duodenum [15-17]. They also provide relief of symptoms caused by these ulcers. In addition, generic PPIs are very cheap in comparison with other anti-ulcer drugs. However, the use of PPIs has been linked to a number of widely publicised side effects in observational studies. These include predisposition to infections by Clostridium difficile and other opportunistic organisms; electrolyte imbalance including low sodium, magnesium, and calcium levels; renal impairment; osteoporosis; and even dementia. These side effects are mostly observed in elderly patients using long-term high dose PPIs, being the very people who are known to be chronic users of NSAIDs and aspirin. Therefore, despite being not fully proven, these side effects cannot be dismissed out of hand or ignored [15].
Alternatives acid inhibitors to PPIs include histamine-2 receptor antagonists, particularly famotidine, or the P-CABs [15,18]. Famotidine has been widely tested in users of aspirin and NSAIDs [15, 17], Figure-1.
However, acid inhibitors cannot heal or prevent aspirin or NSAID-induced ulcers affecting the small bowel or colon, where the pH is alkaline already.
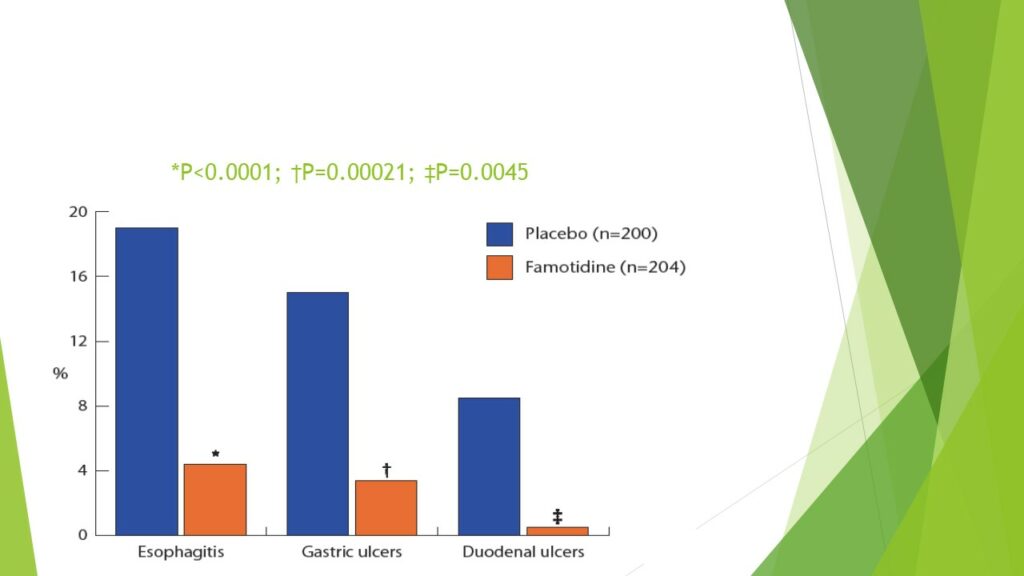
Figure-1: Prevention of aspirin induced ulcers by famotidine 40-mg daily compared to placebo. Famotidine was superior to placebo in the prevention of oesophagitis, gastric, and duodenal ulcers in users of low-dose aspirin. Reference-17: Taha AS at al, Lancet 2009.
Prostaglandin analogues. Misoprostol, a prostaglandin-E1 analogue, has been shown to prevent and heal gastric and duodenal ulcers and erosions in aspirin and NSAID users [16]. More recently, it has been shown to heal small bowel ulcers and erosions caused by these drugs [9], Figure-2. This rather novel activity, like that in the stomach and duodenum, relies on the fact that aspirin and NSAIDs cause GI damage by inhibiting mucosal prostaglandin synthesis. However, misoprostol should not be given to women of child-bearing potential unless they use reliable contraceptive methods.
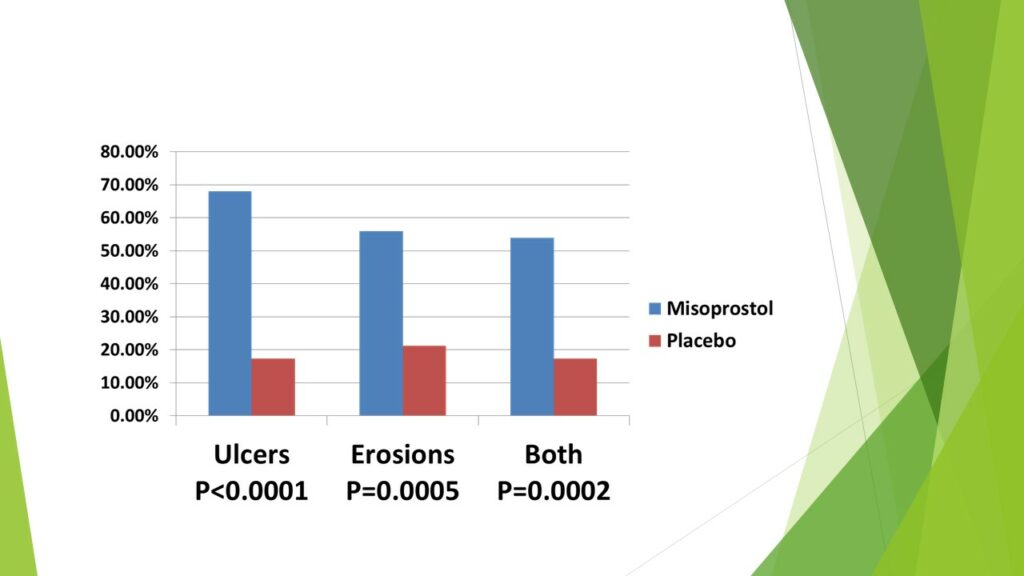
Figure-2. Healing of NSAID induced small bowel ulcers and erosions was significantly greater by the use of misoprostol 200 ug four times daily compared to placebo. Reference-9: Taha AS et al, Lancet Gastroenterol Hepatol 2018.
Combined tablets. Some mucosal protective agents have been combined with NSAIDs in single pills in order to improve compliance with their intake and ensure protection. Examples include Arthrotec(R) (diclofenac plus misoprostol) and Duexis(R) (ibuprofen plus famotidine) [19].
Gut microbiome modification. Intestinal bacteria are known to mediate, at least in part, mucosal damage caused by aspirin and NSAIDs. Recently, it has been shown that Bifidobacterium breve Bif195 protects against small-intestinal damage caused by acetylsalicylic acid in healthy volunteers. This is a promising field which is still under investigation [20].
Other considerations: NSAID related vascular risks. In addition to their well-documented and widely publicised GI side effects, non-aspirin NSAIDs have been linked to increased risk of athero-thrombotic vascular events. The vascular risks of high-dose diclofenac, and possibly ibuprofen, are comparable to coxibs, whereas high-dose naproxen is associated with less vascular risk than other NSAIDs. Although NSAIDs increase vascular and gastrointestinal risks, the size of these risks can be predicted, which could help guide clinical decision making [1].
Conclusions
NSAIDs, including aspirin, are widely used worldwide, and the projection is for their use to continue at this level or even to increase in the coming years. A practical strategy is to use these agents for the shortest duration of time and at the lowest dose possible; to use compounds known to be of low GI and vascular risk; and to co-prescribe PPIs as a first choice, famotidine, or misoprostol, as relevant to the individual patient. Safe clinical practice requires greater awareness of their GI and other side effects, and careful consideration of all of the appropriate preventative and management strategies.
Author Biography

Professor Ali S Taha
Professor Ali S Taha is Consultant Physician & Gastroenterologist at University Hospital Crosshouse, Kilmarnock, affiliated to University of Glasgow. His research interests include mucosal damage and repair and gastrointestinal bleeding in relation to the use of aspirin, NSAIDs, anti-thrombotic agents, acid inhibitors, and prostaglandins.
CME
Pharmacological management of acute upper gastrointestinal bleeding
02 October 2024
Test and treat Helicobacter pylori (HP) in dyspepsia
20 February 2024
- Coxib and traditional NSAID Trialists' (CNT) Collaboration; Bhala N, Emberson J, Merhi A, Abramson S, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382(9894):769-79. doi: 10.1016/S0140-6736(13)60900-9.Ghlichloo I, Gerriets
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs). Ghlichloo I, Gerriets V. Nonsteroidal Anti-inflammatory Drugs (NSAIDs). https://www.ncbi.nlm.nih.gov/books/NBK547742/ Accessed 22/03/2023
- Cleveland Clinic. Antiplatelet drugs. https://my.clevelandclinic.org/health/drugs/22955-antiplatelet-drugs Accessed 22/03/2023
- Rodriguez-Miguel A, Garcia-Rodriguez LA, Gil M, et al. Population-based case-control study: chemoprotection of colorectal cancer with non-aspirin non-steroidal anti-inflammatory drugs and other drugs for pain control. Aliment Pharmacol Ther 2019;50:295-305.
- Kolawole OR, Kashfi K. NSAIDs and Cancer Resolution: New Paradigms beyond Cyclooxygenase. Int. J. Mol. Sci. 2022;23(3):1432; https://doi.org/10.3390/ijms23031432
- Strate LL. Nonsteroidal anti-inflammatory and antiplatelet drugs and the risk of GI bleeding: don’t forget the colon. Gastrointest Endosc 2014;80:1132–4.
- Tibble JA, Sigthorsson G, Foster R, et al. High prevalence of NSAID enteropathy as shown by a simple faecal test. Gut 1999;45:362-366.
- Taha AS, McCloskey C, Craigen T, et al. Occult vs. overt upper gastrointestinal bleeding – inverse relationship and the use of mucosal damaging and protective drugs. Aliment Pharmacol Ther 2015;42:375–382.
- Taha AS, McCloskey C, McSkimming P, et al. Misoprostol for the healing of small bowel ulcers in obscure bleeding related to aspirin and non-steroidal anti-inflammatory drugs (MASTERS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Gastroenterol Hepatol 2018;3:469-76.
- Dydyk AM, Sizemore DC, Haddad LM, et al. NP safe prescribing of controlled substances while avoiding drug diversion. 2023 Jan 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 33232099. https://pubmed.ncbi.nlm.nih.gov/33232099/Accessed 24/03/2023
- Drugs.com. Gabapentin side effects. https://www.drugs.com/sfx/gabapentin-side-effects.html Accessed 24/03/2023
- Chan FK, Lanas A, Scheiman J, et al. Celecoxib versus omeprazole and diclofenac in patients with osteoarthritis and rheumatoid arthritis (CONDOR): a randomised trial. Lancet 2010; 376:173–79.
- Hawkey C, Avery A, Coupland CAC, et al; HEAT Trialists. Helicobacter pylori eradication for primary prevention of peptic ulcer bleeding in older patients prescribed aspirin in primary care (HEAT): a randomised, double-blind, placebo-controlled trial. Lancet. 2022;400(10363):1597-1606. doi: 10.1016/S0140-6736(22)01843-8.
- Rowland M. The continuing decline in the prevalence of Helicobacter pylori Lancet Child Adolesc Health. 2022;6(3):139-140. doi: 10.1016/S2352-4642(22)00026-8.
- Taha AS. Vonoprazan and NSAIDs – New Era in Acid Inhibition and Gastro-protection. Gut 2018;67:995-96.
- Scally B, Emberson JR, Spata E, et al. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: a meta-analysis of randomised trials. Lancet Gastroenterol Hepatol. 2018; 3(4):231-241. doi: 10.1016/S2468-1253(18)30037-2.
- Taha AS, McCloskey C, Prasad R, Bezlyak V. Famotidine for the prevention of peptic ulcers and oesophagitis in patients taking low-dose aspirin (FAMOUS): a phase-III, randomised, double-blind, placebo-controlled trial. Lancet 2009;374:119-25.
- Pomenti S, Katzka DA. Editorial: P-CABs for treatment of reflux oesophagitis—is this the future? Aliment Pharmacol Ther. 2023;57:146–147.
- Taha AS. The ibuprofen–famotidine combined pill – a promise fulfilled. Current Medical Research & Opinion 2015;31: 421–422.
- Mortensen B, Murphy C, O’Grady J, et al. Bifidobacterium breve Bif195 protects against small-intestinal damage caused by acetylsalicylic acid in healthy volunteers. Gastroenterology 2019;157:637–46.
