Author:
Cynthia Kanagasundaram
Acknowledgments:
Dr Pooja Khanna (Gastroenterology Clinical Lead)
Dr Joya Bhattacharyya (Chief Clinical Information Officer, Consultant Gastroenterologist)
Javeria Iqbal (Service Manager, Gastroenterology and Colorectal)
What were the challenges to your service and why did you need to change?
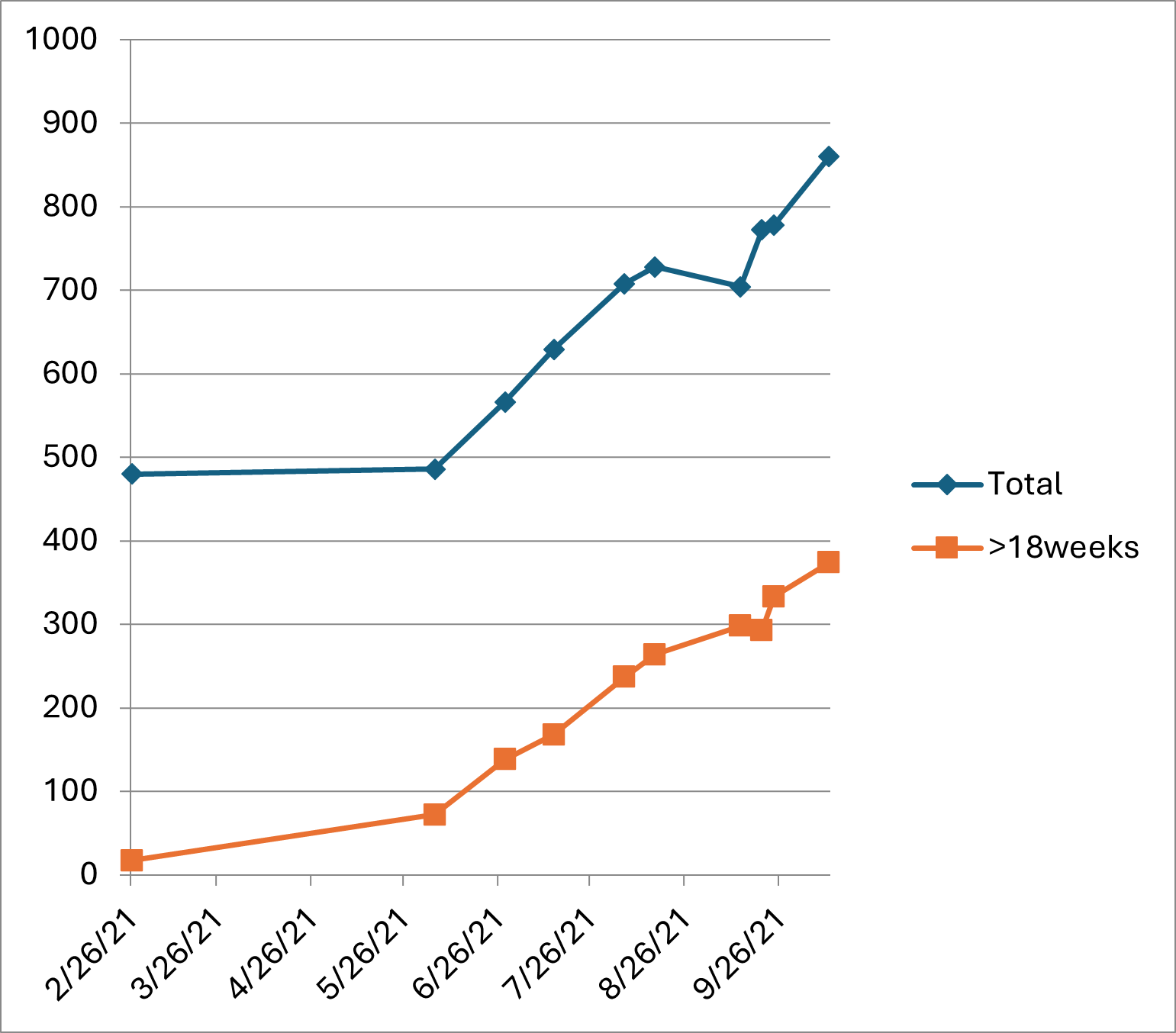
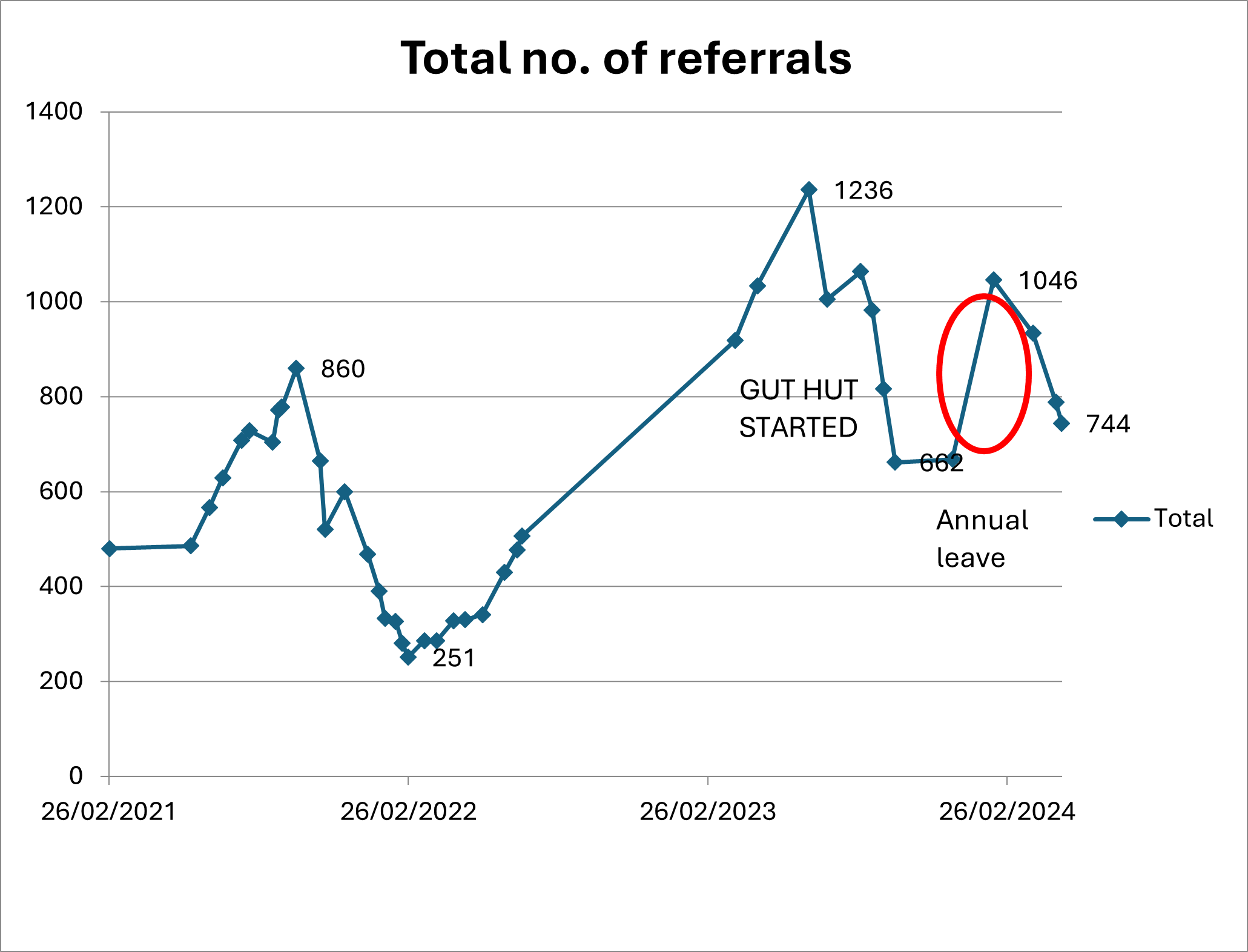
Following the Covid pandemic the gastroenterology waiting list for routine first outpatient appointments continued to grow despite various interventions at attempting to reduce it. The original interventions included changing of clinic templates, increasing locum clinicians and waiting list initiatives. In September 2021 the total number of patients waiting greater than 18 weeks to be seen had peaked at 374 with a total of 860 patients waiting. Despite all these interventions, the waiting list had peaked to 1235 patients in July 2023.
There were also several key events which impacted our ability to reduce the waiting list to include trainee departures in March 2021, which unfortunately we were unable to replace until September 2021. Furthermore, the long-term locum gastroenterologist left the Trust in June 2021 which we were unable to replace and lastly, we encountered difficulties recruiting new consultants into position. Due to the increased turn around in staffing we needed to explore novel strategies to deal with the demands of the increasing waiting list. Further clinic sessions were limited by physical space to do the clinic, expense of setting these up and consultant availability to staff them. In view of this we created a unique triage GUT HUT service with the aim of remotely utilising a consultant in a 1PA capacity to review 30 patients per PA and appropriately triage them to various pathways using created template letters.
Figure 1: Patients waiting greater than 18 weeks and total number of referrals February 2021 to September 2021
How did you overcome the challenges?
An urgent action plan was prepared in February 2023 and thereafter reviewed in April 2023 to provide a detailed roadmap to tackle Gastroenterology new out-patient appointments waiting lists. We named the service GUT HUT, one clinic template had 30 patients which was equivalent to 1PA session where routine gastroenterology referrals were uploaded to a database which I designed, built and implemented.
This database was interrogated by myself and then review the patients case notes and through this triage, patients were either allocated to a straight to test pathway which included to biochemical analysis, endoscopy or imaging and GI investigations or refer them to clinic or discharge them with advice to the GP. For each referral I also created a standard investigation panel to make sure we were uniformed, consistent and offering all patients all the same standard of care.
To enable a safe and effective discharge and follow-up of patients entering GUT HUT, I also created several templates letters outlining details of the patients’ investigations, results and necessarily follow up for both GPs and the patient. For those patient requiring investigations, once these were performed the results would come back to the GUT HUT clinician where further management decisions could be made. All outcomes were coded and uploaded onto our EMR so everything can be tracked and audited.
Importantly patients who were flagged as being frail or had complex medical or surgical histories to include those with inflammatory bowel disease were triaged directly to outpatient to maintain safety.
To aid with the administrative burden of the GUT HUT we employed a PA who would closely liase and work with the managerial team and myself. I was involved in training the PA, supervising them and upskilling them. I was also responsible for auditing the service quarterly to make sure we were delivering an effective initiative.
What were the outcomes?
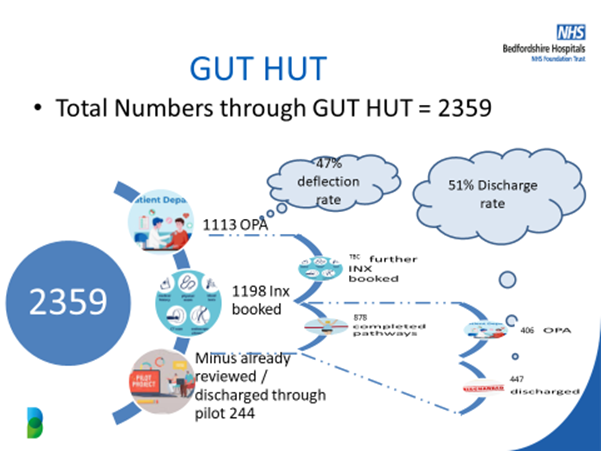
The primary outcome was to reduce the overall waiting lists. In total 2359 patients were reviewed in GUT HUT over an 18-month period, 1113 patients were sent to outpatient clinic which was a 47% decrease in outpatient numbers; 1198 were referred for investigation and 224 were directly discharged. Following investigations a further 447 patients were directly discharged which resulted in an overall discharge rate of 51%. We received no complaints from patients or GPs regarding the safety or effectiveness of the service and our audit showed that the GUT HUT was safe and effective. To highlight the impact of Gut Hut, when the service was paused for a couple of weeks due to annual leave there was an exponential rise in routine OPA.
Figure 2: The impact on Gut HUT on waiting lists.
What were the learning points and how can this influence other teams?
This model of care is a safe and an effective method where patients can be triaged, quickly and appropriately, which results in a decrease in both waiting lists and increase the discharge rate. It is time and cost effective as 30 patients could be explored in a 1PA session which was a 200% increase in capacity of patients from a standard clinic. The Gut Hut service therefore has potential to dramatically reduce waiting lists, offer timely investigations and lead to fast discharge. Furthermore, the generic templates that were built offer detailed explanations to patients and GPs meaning that time could be saved dictating and approving letters that are associated with a standard clinic.
The details regarding the GUT HUT pathway and data were presented to our local GPs and the feedback was well received. We also utilised this opportunity to highlight the importance of including all the relevant information, investigations and if the patient would agree to an invasive investigation such as an endoscopy.
Figure 3: GUT HUT pathway
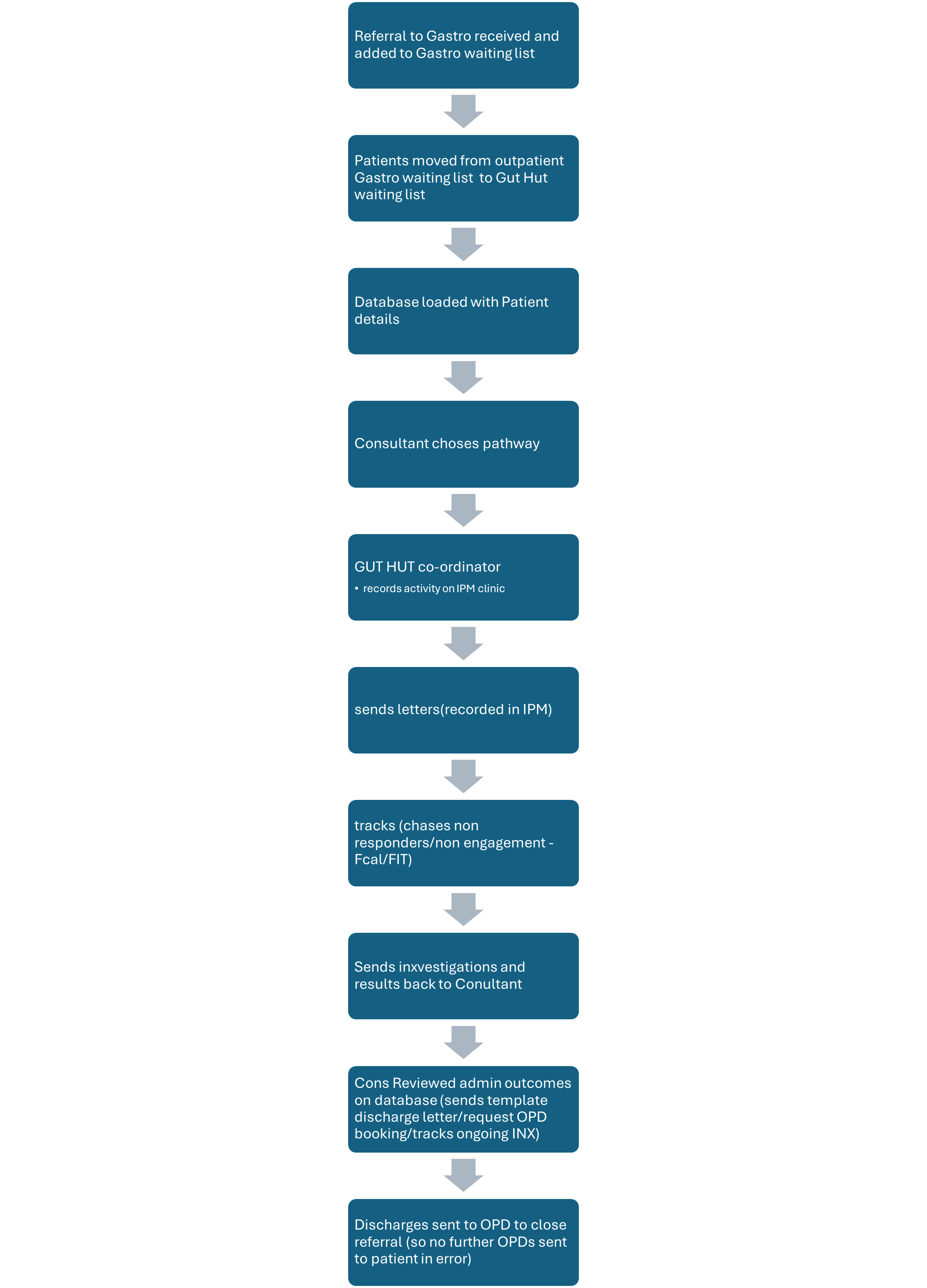
Figure 4: overall outcomes from Gut Hut
Read More

