Author:
Sajjad Mahmood - Consultant HPB Gastroenterologist and advanced endoscopist
Acknowledgments:
Scott Oakes - Gastroenterology ACP
Daniyal Baig - Post CCT fellow in HPB, EUS/ERCP
Diane Wightman - Unit Manager – GI Medicine
Mohamed Korani - Consultant Gastroenterologist
Pawan Lekharaju - Consultant HPB Gastroenterologist and advanced endoscopist
Javaid Iqbal - Consultant HPB Gastroenterologist and advanced endoscopist
Transforming Pancreatic Cyst Surveillance Care
An Innovative ANP-Led Pancreatic Cyst Surveillance Model: Standardising Care, Optimising Resources, and Enhancing Patient Outcomes
Challenges and the Need for Change
Development of the Advanced Nurse Practitioner (ANP)-led Pancreatic Cyst Surveillance Service was driven by critical challenges that highlighted the need for a structured, unified and specialist approach to patient management. Increasing utilisation of cross-sectional imaging had led to a surge in incidental pancreatic cyst detections1, however the lack of a standardised referral pathway meant these cases were often managed inconsistently. An initial service evaluation revealed less than half (47.5%) of a patient sample (40) were undergoing guideline-adherent surveillance, and three different guidelines followed. This lack of uniformity resulted in both under- and over-surveillance, ultimately impacting patient outcomes.
In addition, this also placed significant strain on tertiary Hepato-Pancreato-Biliary (HPB) services. Many patients with incidental cysts were routinely referred to the HPB clinic, where waiting times stretched from 12 to 18 months post-pandemic.
Previous studies indicate that individuals diagnosed with pancreatic cystic neoplasms (PCNs) often feel unsupported and uncertain about their prognosis and next steps2. This underscored the necessity for a dedicated service that could provide guidance, reassurance and a structured care plan.
Surveillance communication, in some cases, relied solely on letters without direct patient interaction, posing a risk of patients feeling disconnected and being lost to follow-up. Conversely, some patients were over-investigated despite co-morbidities.
These issues were further compounded by rising pancreatic cancer incidence and mortality rates3. Some pancreatic cysts have malignant potential, making structured surveillance critical for improving outcomes. Against this backdrop, establishing a dedicated surveillance service was imperative—not only to streamline monitoring and enhance adherence to best practice guidelines but also to improve patient outcomes and experiences.
Overcoming the Challenges
Setting up the service was not without obstacles. Finding appropriate personnel with the necessary expertise was crucial. In this case, the ANP possessed extensive experience working with HPB physicians and surgeons and had undertaken modules in pathology, prescribing, and diagnostics, along with annual Ionising Radiation Medical Exposure Regulations (IRMER) training. The next stage involved negotiating a secure a job plan with dedicated time for the cyst surveillance service.
To gain traction, we needed to drive engagement, initially via a formal inauguration to introduce the service locally and later trust-wide through regional MDT meetings and the MFT (Manchester University NHS Foundation Trust) HPB business forum. This raised awareness and encouraged referrals, reducing reliance on the HPB clinic or fragmented pathways. It was also showcased at the Greater Manchester Cancer Alliance annual conference on 14 May 2024 and the AUGIS (Association of Upper GI Surgeons) annual scientific meeting on 12 September 2024.
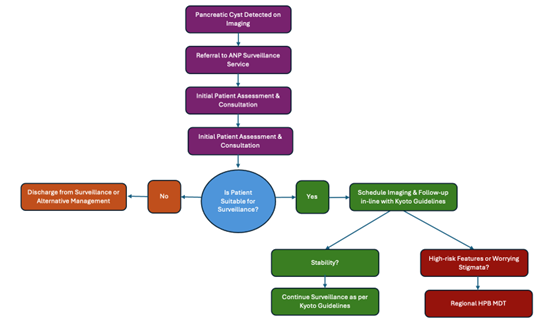
Another challenge was establishing a unified surveillance algorithm. Multiple guidelines existed, creating disparities in follow-up. The European guidelines4 were initially followed, however the team identified the new 'International Evidence-Based Kyoto Guidelines for the Management of Intraductal Papillary Mucinous Neoplasm of the Pancreas'5 as the most comprehensive. These guidelines were formally adopted after presentation at HPB business meeting in March 2024.
To ensure effective tracking and follow-up, robust data collection was essential. A local MFT server enabled the development of a secure spreadsheet to log and monitor patients, improving the understanding of pancreatic cysts' natural history within the local population. Additionally, the service leveraged the capabilities hospitals advanced Electronic Medical Record to streamline administrative tasks, scan requests, team communication, patient tracking and appointment scheduling.
Outcomes
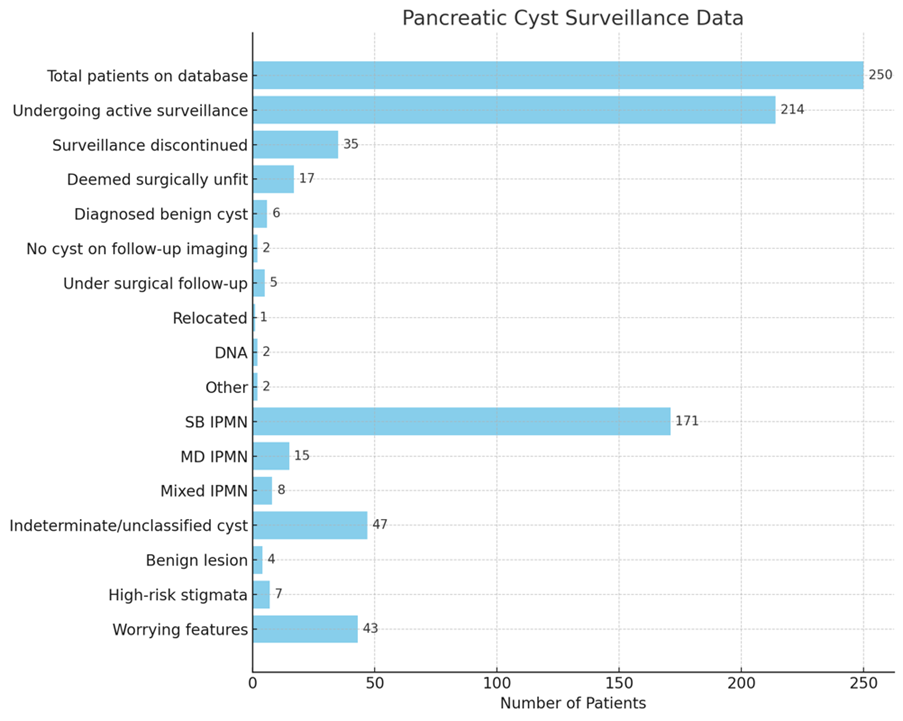
Since inception in April 2023, the service has reviewed 250 patients and delivered 28 clinics, yielding significant clinical, operational, and economic benefits:
- Resource Optimisation (cost savings and Freeing up HPB Consultant clinic slots)
- All patients underwent suitability assessments using both clinical judgment and objective criteria for surgical candidacy.
- Surveillance was appropriately discontinued in 35 cases (14%), including 17 patients (6.8%) deemed surgically unfit (Table 2). This reduction in unnecessary imaging and follow-ups generated significant cost savings. With MRI scans costing approximately £187 and consultant-led appointments averaging £156, discontinuing surveillance in these cases equates to an estimated annual saving of £12,005. Further savings are achieved through ANP-led long-term follow-up in place of consultant-led care, alongside indirect cost reductions in patients overall journeys, which are more challenging to quantify.
- 79 patients previously under the HPB clinic were absorbed by the new service, freeing up slots for other HPB patients.
- Given that each patient required approximately 40 minutes of consultant time annually (imaging reviews, requests, MDT discussions and patient communication) this equated to over 52 hours of consultant time saved per year. This translates to 104 freed up clinic slots (assuming 30 minutes for new appointments).
- Standardisation of Care
- A single, agreed-upon protocol was applied, reducing variability in follow-up.
- High Patient Engagement
- Only 2 patients (0.8%) failed to engage with the surveillance, demonstrating the services success in patient tracking, communication, and engagement.
- Centralised, Specialised, Single-Point of Contact
- 112 referrals came from non-HPB specialties, now receiving dedicated care.
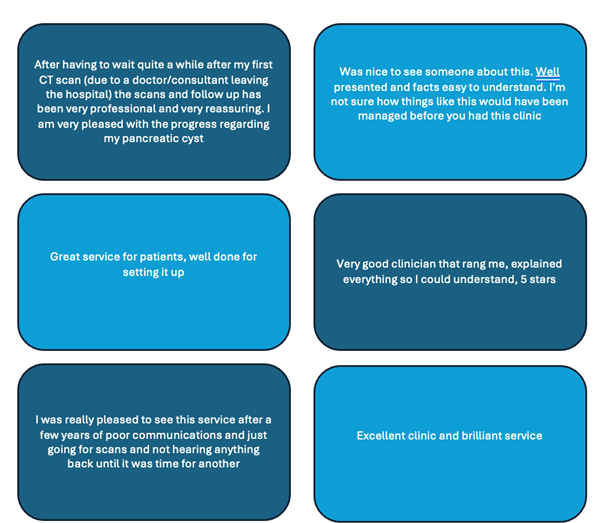
- Positive Clinician and Patient Feedback
- Clinician and patient feedback were overwhelmingly positive, with 90% of surveyed patients reporting a better understanding of their cyst and surveillance plan (figure 2).
Key Takeaways
- Dedicated Specialised Service Improves Outcomes
- A unified surveillance protocol reduced variability and ensured consistent, high-quality patient care.
- Structured database facilitated robust data collection, contributing to the growing knowledge base on pancreatic cyst management.
- Patient-Centred Communication Enhances Engagement
- Moving away from generic correspondence to personalised consultations improved patient understanding and satisfaction (figure 2).
- Empathetic, tailored communication fostered trust and adherence to surveillance plans.
- Proactive Discharge Strategies Optimise Resources
- Regular case reviews ensured patients no longer needing surveillance were discharged, balancing efficiency with patient safety and ensuring appropriate resource allocation.
References
- Heyn, C., Sue-Chue-Lam, D., Jhaveri, K. & Haider, M.A., 2012. MRI of the pancreas: Problem-solving tool. Journal of Magnetic Resonance Imaging, 36, pp.1037–1051.
- Reeve, R., Foster, C. & Brindle, L., 2024. Exploring patient experiences of surveillance for pancreatic cystic neoplasms: A qualitative study. BMJ Open Gastroenterology, 11, e001264. doi:10.1136/bmjgast-2023-001264.
- Ilic, I. & Ilic, M. (2022). International patterns in incidence and mortality trends of pancreatic cancer in the last three decades: A joinpoint regression analysis. World Journal of Gastroenterology, 28(32), 4698 – 4715.
- European Study Group on Cystic Tumours of the Pancreas. (2018) European evidence-based guidelines on pancreatic cystic neoplasms. Gut, 67(5), pp. 789–804. doi:10.1136/gutjnl-2018-316027.
- Tanaka, M., Fernández-Del Castillo, C., Kamisawa, T., Jang, J.Y., Levy, P., Ohtsuka, T., Salvia, R. & Shimizu, Y., 2024. International Evidence-Based Guidelines for the Management of Intraductal Papillary Mucinous Neoplasm of the Pancreas (Kyoto Guidelines). Pancreatology, 24(1), pp.1–15. doi:10.1016/j.pan.2024.01.001.
- NHS England. (2023) 2023–25 NHS Payment Scheme. Available at: https://www.england.nhs.uk/publication/2023-25-nhs-payment-scheme/ (Accessed: 3 February 2025).
Read More

