Author:
Dr Rebecca Grant
Acknowledgments:
Dr Will Brindle - Consultant gastroenterologist
Dr Rahul Kalla - Consultant gastroenterologist
Dr Gail Masterton - Consultant gastroenterologist
Professor John Plevris - Consultant gastroenterologist
Dr Colin Noble - Consultant gastroenterologist
Dr Eleanor Watson - Consultant gastroenterologist
Dr Ian Penman - Consultant gastroenterologist
Dr Nick Church - Consultant gastroenterologist
Dr Ben Shandro - Consultant gastroenterologist
Dr Aaron McGowan - Consultant gastroenterologist
What were the challenges to your service and why did you need to change?
In 2020 endoscopy services in NHS Lothian (as in the rest of the country) were coming under increasing pressure, this was then exacerbated by the advent of the COVID-19 pandemic. It was therefore essential to reduce demand on stretched services and to facilitate shorter waiting times for high yield investigations. The performance of repeat oesophagogastroduodenoscopies (OGDs) to assess for healing of gastric ulcers 6-8 weeks after the index procedure was highlighted as a potential area for change. Despite current British Society of Gastroenterology guidelines recommending this practice, evidence favouring it is relatively weak and largely historical, with the majority of recent studies demonstrating that a combination of histology and benign appearances at endoscopy are sufficient to exclude malignancy.
How did you overcome the challenges?
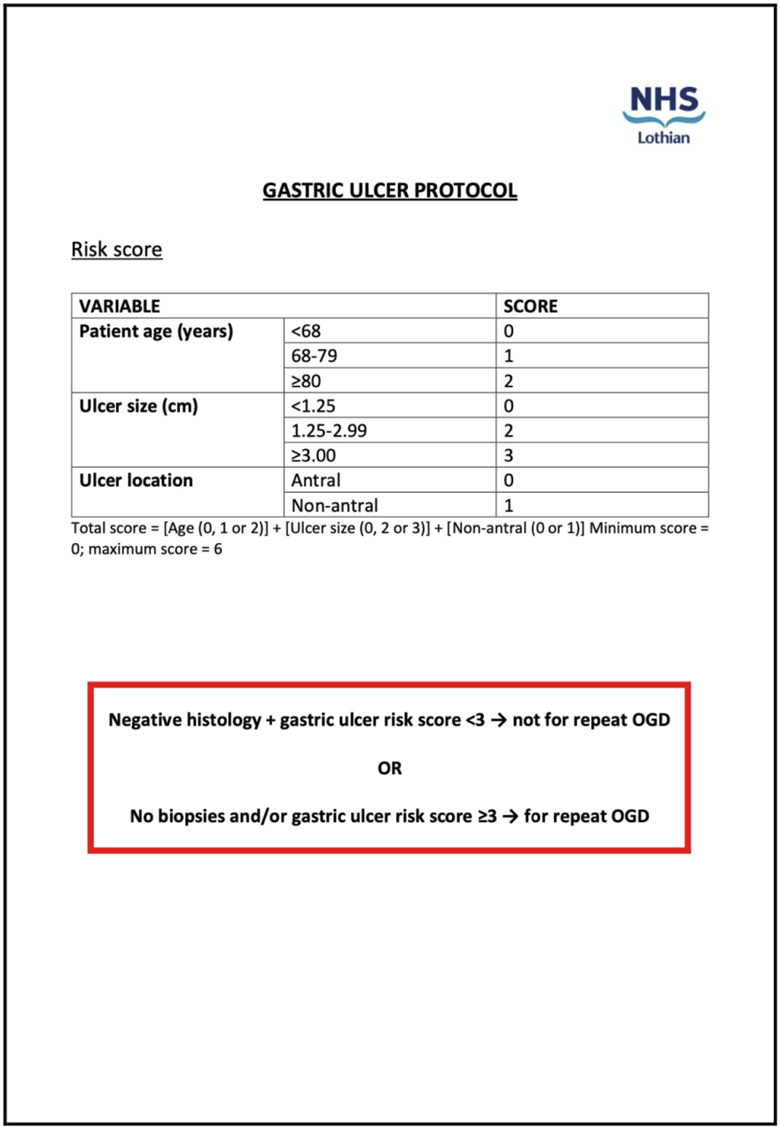
We identified 778 patients who had been diagnosed with a gastric ulcer in NHS Lothian between 1st January 2014 and 31st December 2018. All patient records were then reviewed to determine if there were factors at the index OGD which were significantly associated with a diagnosis of gastric cancer. Older patient age (p=0.014), increased ulcer size (p<0.001) and a non-antral ulcer location (p=0.030) were significantly associated with malignancy on multivariable regression analysis and were used to form the basis of a risk score to identify patients at greatest risk of gastric cancer (and therefore warranting a repeat OGD). The risk score produced a negative predictive value of 97.4% in the NHS Lothian derivation cohort and of 98.6% in an external validation cohort in Leeds.
In combination with subsequent histology results, the risk score was used to create an algorithm to risk stratify patients for repeat OGDs. This algorithm was adopted as the new gastric ulcer protocol in hospitals across NHS Lothian in May 2021 (Figure 1). The protocol was reviewed by our clinical management team and approved for implementation within our health board. Working with our management team, we developed an SBAR (Situation, Background, Assessment and Recommendation) summary for our new protocol. To ensure awareness of the change in practice, all endoscopists were informed by email, presentations were conducted at hospital sites within the health board and posters were provided to be displayed in all endoscopy rooms.
What were the outcomes?
Protocol outcomes have been assessed since its adoption in May 2021 to determine if there have been any missed gastric cancer diagnoses in patients since implementation and at follow-up. We identified 236 patients diagnosed with a gastric ulcer between 24th May 2021 and 24th June 2023. The index and (if relevant) repeat OGD results for these patients were reviewed, in addition to all clinical correspondence, notes and results for any subsequent diagnoses or investigations for gastric cancer (median follow-up time of 22 months (interquartile range (IQR) 17-27 months).
In total, 73.2% of decisions regarding follow-up OGDs (both to perform and not to perform) were made in accordance with the protocol. No new pathology was diagnosed at repeat OGDs which were performed contrary to the protocol. Crucially, at the median follow-up time of 22 months there were no missed gastric cancer diagnoses in patients that the protocol advised to not have a repeat OGD.
At an approximate cost of £471.00 per procedure (based on national tariffs), savings may be estimated at £45,216 (96 OGDs) in not performing repeat OGDs over the course of our follow-up study (or £22,608 annually (48 OGDs). However, if the new ulcer protocol was followed for all patients, £63,114 (114 OGDs) would have been saved over the course of the study (£31,557 (67 OGDs) annually).
What were the learning points and how can this influence other teams?
- The NHS Lothian Gastric Ulcer Protocol is a safe and effective method to reduce the burden of repeat OGDs on both patients and on endoscopy units.
- Crucially, protocol adherence has demonstrated no missed gastric cancer diagnoses.
- Work on protocol awareness amongst staff is ongoing, with staff being kept up to date on the results of ongoing monitoring of the protocol. The positive results that we have produced so far are helping to contribute to a gradual change in practice.
- There is potential for endoscopy units to make significant cost savings and to allow more resources to be directed towards high-risk patients.
- A reduction in the number of OGDs performed may also positively contribute to sustainability in endoscopy.
Figure 1: NHS Lothian Gastric Ulcer Protocol
Read More

