Authors:
Stacey Munnelly and Alex Hadall, Advanced Nurse Practitioners in Gastroenterology
Acknowledgements:
Roja Thananki Gastro, Advanced Nurse Practitioner, and Dr Joe Geraghty, Consultant Gastroenterologist/Clinical Supervisor
Success Story
Pancreatitis is a painful devastating illness that requires a specialist multidisciplinary team (MDT) approach to care. However, a UK National Confidential Enquiry into Patient Outcome and Death (NCEPOD) found NHS care for pancreatitis to be inadequate and inequitable, demonstrating patients can struggle to receive treatment and support (O’Reilly et al, 2016). Following the enquiry, formalised regional tertiary ‘hub and spoke’ networks were recommended, so that all patients can access specialist pancreatitis care irrespective of which hospital they present to.
Manchester University NHS Foundation Trust (MFT) is an established tertiary pancreatitis hub. Patient cases are referred to the benign Hepato-Pancreato-Biliary (HPB) MDT from surrounding hospitals. The MDT offer specialist opinion on the management of pancreatitis and a range of radiological, endoscopic, and surgical interventions for complications. Patients experiencing severe complex pancreatitis are transferred from across the region and can spend weeks to months receiving in-patient care. Such severe illness demands support for the physical recovery, but also for the psychological impact of the disease beyond discharge from hospital (Ma et al, 2022). Gaps in service provision were identified through patient feedback and internal service review. Timely follow up and access to help with complex issues after discharge were unavailable. There was an average waiting time of eight months for routine consultant follow up clinic appointments. Limitations in clinic capacity resulted in delays in patients undergoing follow up and treatment. There was also a lack of specialist nursing support for patients with benign pancreatic disease.
The MDT recognised a need to provide accessible timely care for patients with pancreatitis. Three Gastroenterology Advanced Nurse Practitioners (ANP’s) experienced in managing severe complex pancreatitis developed a nurse led service in April 2021. The ANP’s can assess, diagnose, and prescribe treatments and facilitate admissions. They support patients during admission. On discharge an SOS hotline number and email address are provided. Daily hot clinics provide urgent clinical review as required. Follow up clinic appointments are scheduled within two weeks post hospital discharge. Long term follow-up care is provided for patients with chronic pancreatitis. An evidence-based protocol was created to structure the clinical review using guidelines from the National Institute of Health and Care Excellence (NICE) (2020) and European Society of Clinical Nutrition and Metabolism (ESPEN) (Arvanitakis et al, 2020). The ANPs run three routine clinic sessions per week. Stable patients are given the option of telephone or face to face clinics. Clinical supervision is provided by the Gastroenterology/HPB Consultants.
At the end of year one, audit revealed 565 clinic appointments had been conducted. Thirty-four emails and 76 helpline phone calls were responded to. The frequency of emails and calls has steadily increased as more patients have been informed about the service. Now, there are an average of ten calls and four emails per week, leading to hot clinic review. Currently there are 236 outpatients receiving routine follow up, covered by 15 clinic slots per week.
Patient and Consultant feedback was sought through electronic survey. Seventy eight percent of patients agreed they were aware of how to contact the team for support. Patients were asked where they would previously have sought help. Thirty percent said they would have attended the emergency department, 25% would have contacted their GP, 30% would have tried their consultant’s secretary and 15% would have turned to alternative sources including the internet and support groups. One hundred percent agreed they felt supported by the service. Seventy-seven percent said they felt involved in the management of their illness. Ninety-nine percent agreed they received information about their illness. Sixty-six percent of patients felt their pancreatitis was adequately managed by the nurse led service and 33% were undecided. Seventy-seven percent agreed that the telephone clinic interferes less with work, family, and social life. One hundred percent agreed the telephone clinic saved on transport costs. However, 11% said they would prefer to be reviewed face to face and 55% were undecided. Patient’s comments explaining the responses to questions and Consultant feedback has been positive describing the impact of the service (Figure’s 1 & 2.)
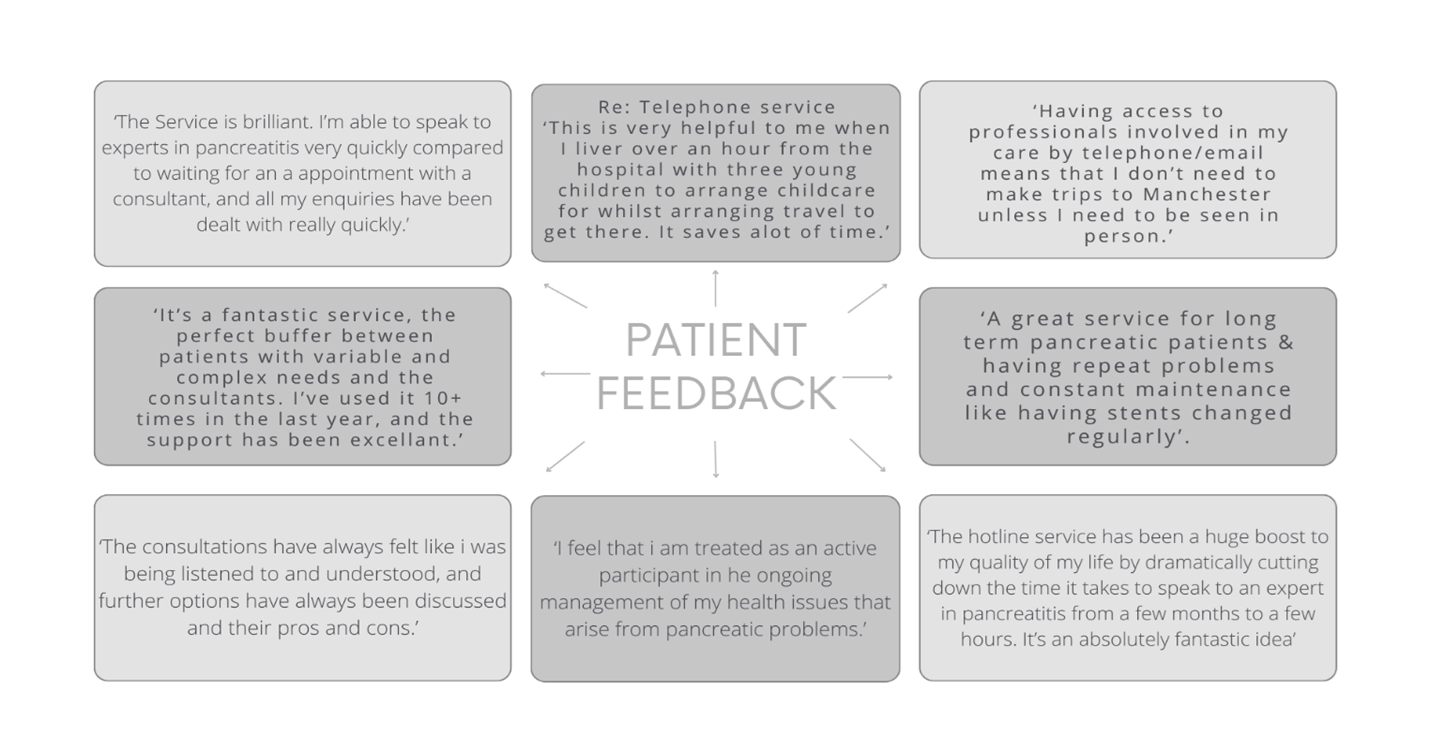
Figure 1.
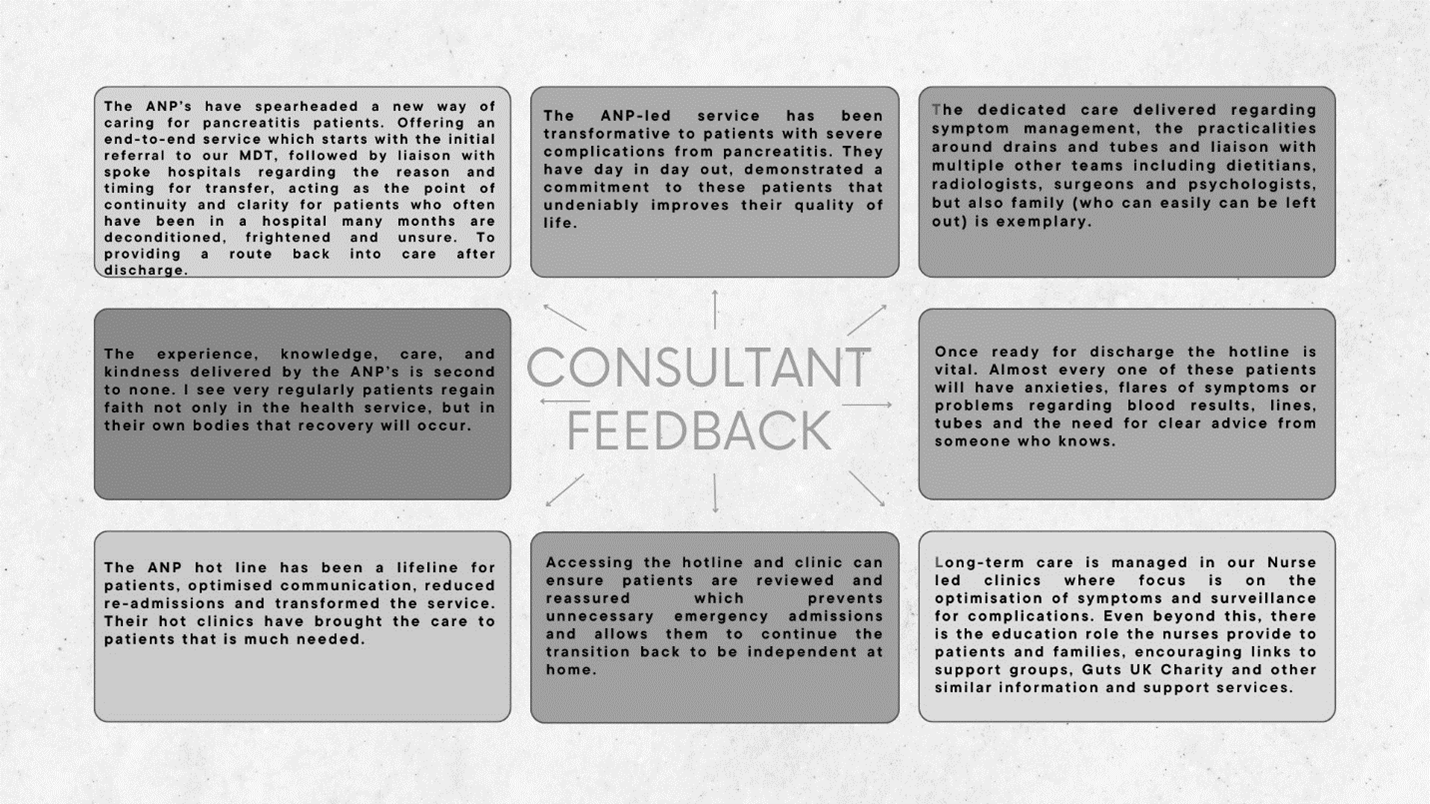
Figure 2.
The NHS long-term plan (NHS England, 2019) emphasises how ANP’s can play a key role in transforming service delivery to better meet local health needs, by providing enhanced capacity, capability, and efficiency within multi-professional teams. The ANP pancreatitis service delivers in this way and achieves national recommendations for tertiary pancreatitis care. The service provides co-ordination and continuity of care in a team with rotating Consultants. Being involved in the whole patient journey, from referral to the MDT, liaising with referring teams, facilitating safe transfer, and providing bedside inpatient care, allows for trusting relationships to form between the nurses, patients, and families. By providing timely follow up and SOS access, prompt assessment and treatment can occur, ensuring patients are managed safely. This accessible specialist care reduces patient discomfort, helps to avoid attendances to the emergency department and improves their experiences. The use of an evidence- based protocol has standardised a holistic approach to pancreatitis care, ensuring symptoms are managed, screening for complications is performed and psychological support is offered. This is important as adherence to evidence-based recommendations for clinical care is associated with better clinical outcomes and lower resource use for patients with chronic diseases (McBrien et al., 2018). Furthermore, learning from this service has been shared with referring teams and specialist nurses across the region to set up local evidence based chronic pancreatitis clinics. Future plans include the pilot of admission and discharge bundles that could be used across UK pancreatitis centres.
References
- Arvanitakis, M. et al., 2020. ESPEN Guideline on Clinical Nutrition in Acute and Chronic Pancreatitis. Clinical Nutrition, 39(3), pp.612–631. Accessed https://www.clinicalnutritionjournal.com/article/S0261-5614(20)30009-1/fulltext
- Health Education England. Multi-Professional Framework for Advanced Clinical Practice in England. 2017. multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (hee.nhs.uk) (accessed 6 February 2024)
- Ma, S, Yang, X, He, H, Gao, Y, Chen, Y, Qin, J, Zhang, C, Lu, G, Gong, W, Chen, W, Ren, Y. (2022). Psychological experience of inpatients with acute pancreatitis: a qualitative study. British Medical Journal Open. 29;12(6):e060107. doi: 10.1136/bmjopen-2021-060107. PMID: 35768082; PMCID: PMC9244672.
- McBrien, K., Ivers, N., Barnieh, L., Bailey, J., Lorenzetti, D., & Nicholas, D. et al. (2018). Patient Navigators for People with Chronic Disease: A Systematic Review. PLOS ONE, 13(2), e0191980. https://doi.org/10.1371/journal.pone.0191980
- National Institute for Health and Care Excellence. (2020) Pancreatitis. Retrieved 6th April, 2022, from https://www.nice.org.uk/guidance/ng104/chapter/Recommendations
- NHS England (2019). The NHS Long Term Plan. www.longtermplan.nhs.uk (accessed 16 February 2024)
- O’Reilly, D, A., McPherson, S, J., Sinclair, M, T., Kelly, K., Ellis, D., Mahoney, N., Smith, N., & Mason, M. (2016) Treat the Cause: A review of the quality of care provided to patients treated for acute pancreatitis. National Confidential Enquiry into Patient Outcome and Death.
Read More

