Authors and acknowledgements:
Abhirami Gautham, James Sun, Eimir Bourke, Milda Reju, Michael Louise Cervantes, Jayshri A Shah
What were the challenges to your service and why did you need to change?
Northwick Park Hospital serves an ethnically diverse population in the London boroughs of Brent and Harrow. Brent, being the 10th most deprived borough in London, has a high burden of liver disease, which is associated with significant healthcare resource utilisation, morbidity and mortality. A GIRFT review conducted in 2023 showed that the emergency liver-admission rate at our trust was 41.6%, which is significantly higher than the benchmark of 37.2%.
A review of electronic patient records (EPR) from August to October 2023 using liver disease-related ICD-10 codes revealed 58 liver-related admissions to the gastroenterology ward. The average length of stay (LOS) was 10.52 (SD = 14.89) days. Given that an average medical bed in our trust costs £257.00 per day, liver-related admissions to the gastroenterology wards costed the trust an average of £2,703.64 per admission from August to October 2023.
We identified that the monitoring of stable in-patients for biochemical improvement or optimisation of medication were potential reasons for increased LOS. Clinicians were reluctant to discharge patients early given the average waiting times for routine outpatient clinic appointments were six-to-eight months. Furthermore, there was difficulty accommodating urgent follow up within four weeks for liver outpatients who required frequent monitoring, resulting in emergency admissions. This review highlighted the need for a strategy which tackled the significant resource and cost associated with the high burden of liver disease in our trust.
How did you overcome the challenges?
We implemented a HOT liver clinic to review patients following inpatient admission or outpatient review. The primary aim of this clinic was to reduce LOS amongst liver patients by providing early clinical review and to minimise emergency admissions amongst liver outpatients.
Patients could be referred following inpatient admission or review in liver outpatients. A standard operating procedure was developed, specifying the following inclusion criteria:
- Patients with cirrhosis who presented with decompensated disease.
- Patients presenting with an acute hepatitis with stable liver function for ongoing review.
- Patients requiring monitoring following commencement or dose adjustment of drugs such as diuretics or immunosuppressants.
The following referrals were deemed inappropriate for the HOT liver clinic:
- Two-week wait referrals to hepatology services from primary care.
- Patients with deranged liver enzymes needing hepatology input from acute medicine, the emergency department or primary care.
- Patients with new decompensated liver disease requiring admission.
- Patients requiring inpatient management of co-existing or related conditions.
- Frail or non-ambulant patients unable to attend for repeated visits.
To streamline patient referrals and ensure optimal care, a HOT clinic referral form (Figure 1) was implemented. This form captured precise information regarding the urgency, clinical details, and desired outcome from HOT clinic review. In addition, an information leaflet was developed to aid patient understanding of the process.
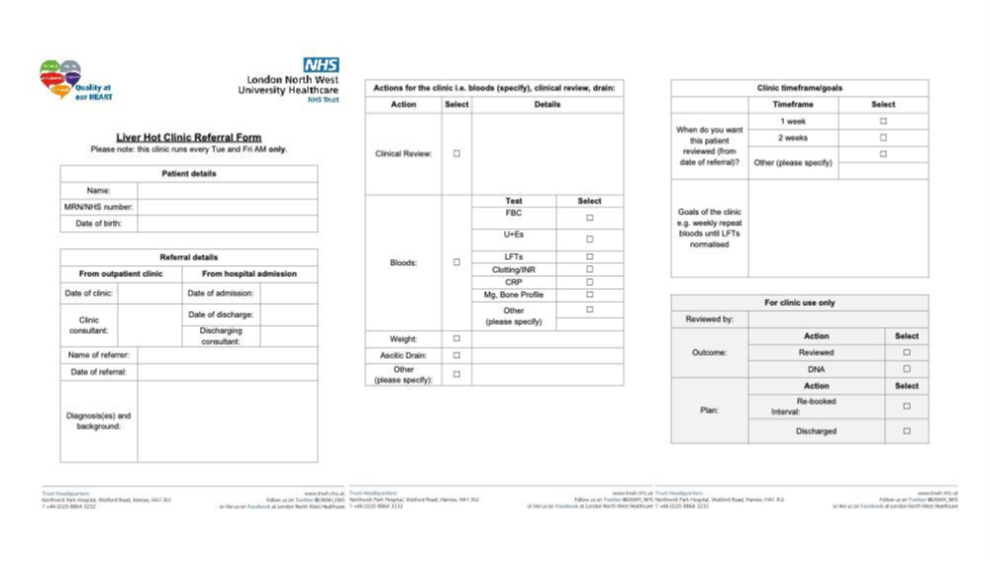
Figure 1. HOT liver clinic referral form.
Two specialist nurses were appointed to support the HOT clinic amongst broader hepatology initiatives. The clinic ran twice weekly in a dedicated clinic room on the gastroenterology ward. During the appointment, patients underwent clinical review by a gastroenterology registrar, supported by the specialist nurse. All clinical decisions were overseen by the ward hepatology consultant. Stable patients requiring no further monitoring were discharged with follow-up in a liver outpatient clinic. Stable patients requiring further optimisation were given further HOT clinic appointments. Patients requiring admission were admitted directly to the gastroenterology ward through liaison with the ward nursing team if possible. Otherwise, admission was organised via the acute medical take. An audit trail of referrals, reviews, admissions and missed appointments was maintained by the specialist nurses.
What were the outcomes?
The flow of patients through the HOT clinic is shown in Figure 2.
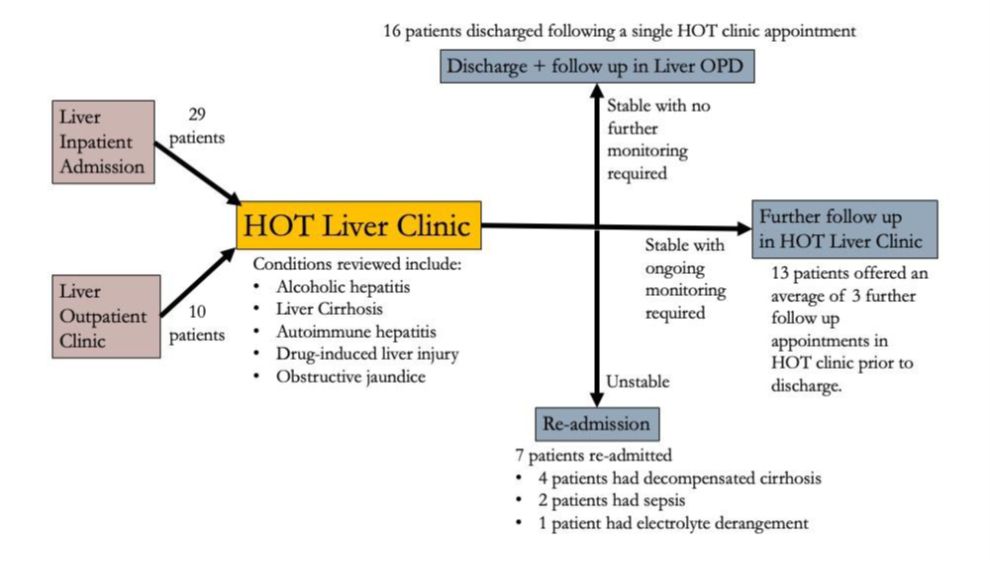
Figure 2. Flow of patients through HOT liver clinic
A total of 39 unique patients were reviewed across 78 appointments. 29 patients were referred following inpatient admissions, while 10 were referred from outpatient clinics. The most common diagnosis was alcohol-related liver disease (23 out of 39 patients, 58.99%). 10 (12.82%) appointments were missed. The mean time to review in the HOT clinic was 13.52 (SD = 8.52) and 26.44 (SD = 23.29) days for patients referred from inpatient admission and outpatient clinics respectively. Of the patients referred from inpatient admissions, 7 (24.14%) were re-admitted to hospital within a three-month period. Four of these patients were admitted directly to the gastroenterology ward from the HOT clinic. The most common cause of readmission was decompensated cirrhosis (4 out of 7 patients, 57.15%). Patients were re-admitted an average of 19.14 (SD = 11.10) days following initial discharge from hospital.
We conducted a further review of EPR to identify liver-related admissions to the gastroenterology wards, from November 2023 to January 2024, following commencement of the HOT clinic. 62 patients were admitted to the gastroenterology wards with liver disease in this period. We compared LOS before and after the introduction of the HOT clinic using an independent samples t-test with unequal variance. This showed a statistically significant reduction in LOS (t = 2.880, p = 0.003) by 6.00 (SE = 2.08) days. A graphical depiction, alongside the mean, median minimum and maximum LOS in both groups is shown in Figure 3. Applying the same cost of an average medical bed as above, liver-related admissions to the gastroenterology wards cost the trust an average of £1,161.64 per admission from November 2023 to January 2024, reflecting mean savings of £1,542 per admission since the implementation of the HOT clinic.
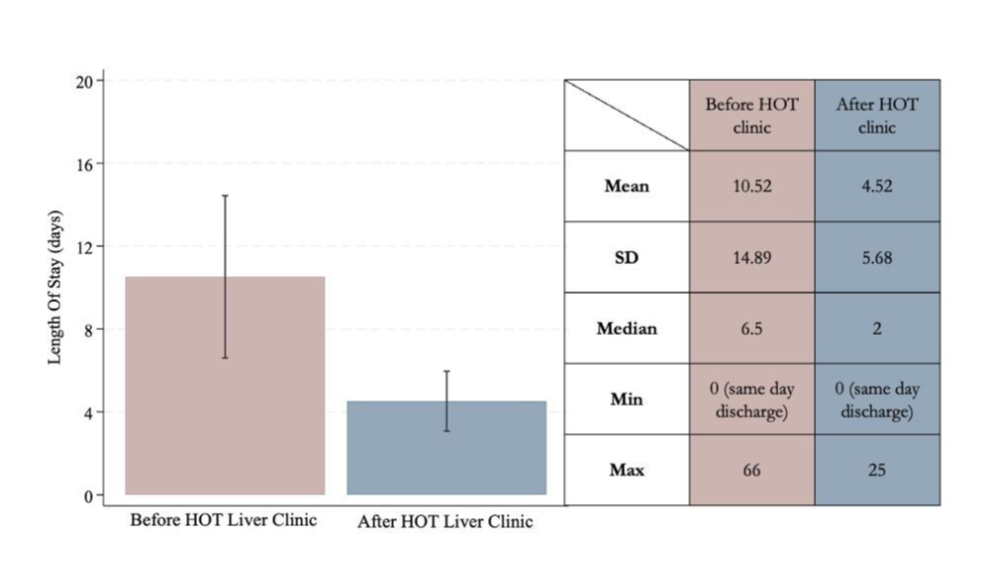
Figure 3. Box Graph of Mean Length of Stay (LOS) and summary of mean, standard deviation (SD), median, minimum and maximum LOS before and after the implementation of the HOT liver clinic.
What were the learning points and how can this influence other teams?
The HOT liver clinic tackles the high burden of liver disease in our trust using a two-pronged approach:
- It supports liver outpatients with timely monitoring and proactive intervention, addressing potential issues before they lead to hospital admission. This reduces long waiting times for those who truly need inpatient care and reduces the need for emergency admissions.
- It provides an invaluable opportunity for post-discharge review, identifying unwell patients who might require swift re-admission. This proactive approach has optimised inpatient resources, significantly reducing costs associated with liver disease in a trust facing high disease burden.
The positive impact described in this report can influence other teams to implement a similar strategy to manage the needs of local liver patients, particular in deprived areas with high disease burden.
Read More

