Authors and acknowlegments:
James J Sun, Kelcy Salinas, Aya Al-Hasani, Anees Fatima, Abhirami Gautham, Gabriel Wallis, Nina Stafford, Jason Salinas, Siv Venkateshwaran, Vicki Timms, Laurence John, Jayshri A Shah
What were the challenges to your service and why did you need to change?
The incidence of morbidity from liver disease is rising in the United Kingdom but the number of Hepatologists has not kept pace with this increase in clinical demand. Chronic hepatitis B (CHB) infection which can progress to liver cirrhosis and therefore patients require monitoring even if asymptomatic carriers. This usually takes place in specialist outpatient clinics. In 2023 our trust had 501 CHB patients on anti-viral therapy and an additional approximately 300 asymptomatic carriers.
This vast amount of CHB patients could not be managed in our pre-existing service where CHB patients would be seen by Hepatology and Infectious Disease Consultant Physicians. 103 (52%) existing Hepatitis B patients on treatment were not allocated to a named Consultant due to retirements. 35% of patients on anti-viral therapy had breached the monitoring guidelines.
Additionally, we implemented NHS blood borne virus (BBV) screening initiative for all patients attending the Emergency Department in May 2022. An audit of the period May 2022 – June 2023 demonstrated that 333 new patients with Hepatitis B (excluding those with a known diagnosis) were identified by BBV screening. This amounts to approximately 25 new patients per month requiring review in a Hepatitis B clinic.
The waiting time for a newly identified Hepatitis B patient to see a clinician was 6-8 months. The demands on the service were compounded by the burden of a significant number of wasted appointments; 19% of consultant appointments for CHB patients were not attended.
How did you overcome the challenges?
To address these challenges, we performed a thorough review of our service provision for CHB patients. Following this we developed two new clinics to tackle the increased number of CHB patients (Figure 1). Both new clinics had clear standard operating procedures stating inclusion and exclusion criteria.
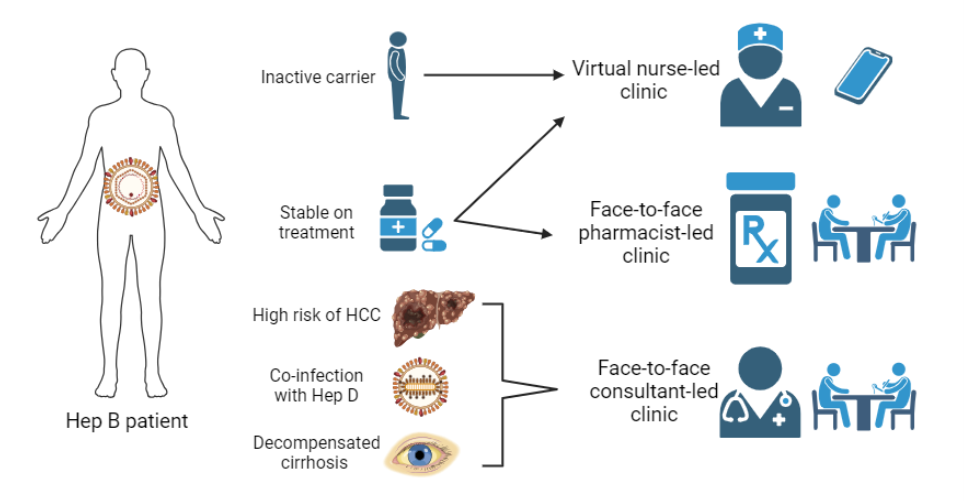
Figure 1: Multidisciplinary approach to Hepatitis B with two new clinics set up to overcome the challenges of patient volume (virtual nurse-led and face-to-face pharmacist-led).
As part of the review process, we studied the non-attendance rates of existing clinics to try to understand patterns and ways of increasing patient engagement. The cost of a missed NHS appointment is £120. We identified appointments in the summer months (July – September) as having the lowest attendance rate (76%). Patients who were not on treatment had a lower attendance rate (79%) compared to those who were (91%). We are now investigating ways of targeting reminders to patients not on treatment and for appointments scheduled over the summer.
What were the outcomes?
Since the implementation of the virtual nurse-led and face-to-face pharmacist led clinic, the waiting time for a new Hepatitis B patient to see a clinician has been reduced to 3 months (Figure 2).
The non-attendance rate to the new clinics were lower than to the Consultant-led clinics. For the Pharmacist-led clinic it was 16% and Nurse-led clinic it was 4%. Consultants and pharmacists conducted almost entirely face-to-face appointments compared to nurse appointments which were virtual. In combination, the odds ratio for non-attendance to face-to-face appointments was 5.00 (95% CI 2.00 – 12.5, p<0.001).
In the new Pharmacist-led clinic interventions performed were able to improve the care patients received: 64% of patients received lifestyle advice, 90% were screened for drug-drug interactions and 24% were identified as meeting criteria for hepatocellular carcinoma surveillance that had not had up-to-date liver imaging.
Figure 2: Waiting time for new appointment
During a one-year period (Jan 2023 – Dec 2023) 117 patients were offered an appointment in the virtual nurse-led clinic and 108 patients were offered an appointment in the pharmacist-led clinic. This freed up 225 Consultant appointments in the first year. Through stratifying patients into the appropriate clinic within our multidisciplinary service we have been able to deal with the challenge of the greatly increased Hepatitis B patient numbers following the introduction of BBV screening.
What were the learning points and how can this influence other teams?
Specialist nurses and pharmacists can support Consultant Physicians in the delivery of Hepatitis B services. The implementation of our multi-disciplinary service has been an effective strategy to increase the availability of clinic appointments.
Overall care of patients with hepatitis B was optimised. By stratifying patients into the different clinics, more complex and high-risk patients could be seen in the Consultant-led clinic where there was a reduction in waiting time for new appointments.
Studying the factors relating to non-attendance of clinic appointments can provide an insight to form the basis of further service development. This can lead to a more efficient clinical service with less wastage from missed appointments.
Read More

