Authors:
Bethan Potter, Endoscopy Lead Nurse
Lindsey Howlett, Service Manager
Karen Mol, Assistant Service Manager
Dominic Bullas, Consultant Gastroenterologist
Elmuhtady Said, Consultant Gastroenterologist
Endoscopy department, Barnsley Hospital NHS Foundation Trust
What were the challenges to your service and why did you need change?
In response to the unprecedented challenges posed by the COVID-19 pandemic, our Endoscopy service undertook a transformative initiative to address the backlog resulting from the loss of elective endoscopic capacity and pre-assessment clinic provision. Our elective capacity was further constrained by workforce limitations (such as protracted absence due to illness, retirement, or endoscopists leaving the department), and nursing and administrative processes that were largely paper-based with all of the inefficiencies that that entails.
Traditional paper-based endoscopy referrals, originating from diverse sources (i.e. a mixed population of clinicians who were either familiar with the endoscopic process or those from specialities not in any way associated with endoscopy), presented differing levels of clinical experience. Owing to the variable quality of the referrals, this placed further demands on the administrative staff who were compelled to pursue referring clinicians for critical information that may have been omitted from the index referral.
Robust clinical oversight and vetting of submitted referrals for endoscopy (across multiple domains of referral: inpatient/outpatient, surveillance and direct access) was sub-optimal, inconsistent, and introduced much delay in the booking of procedures. Additionally, the evolving evidence base and consensus statements relating to endoscopic practice led to the perception that guidelines were not easily accessible or not in routine clinical practice. As a consequence, adherence to nationally-approved BSG guidelines during the process of referral was not universally understood or enacted, leading to cancelled procedures, further delay and a poor patient experience.
How did you overcome the challenges?
The challenges faced by our Endoscopy service prompted the need for a wholesale restructuring of the clinical and administrative process. This was achieved by aligning the wealth of clinical and non-clinical experience in our department with a relentless approach to innovation in process, job planning, clinical engagement, training and technology.
This transformation was borne from a close collaboration within the Multi-Disciplinary Team. This involved gastroenterologists, senior nursing and administrative staff, the operations team and those responsible for cancer and surveillance pathways.
A bespoke, Trust-wide, web-centric digital referral platform was developed, consolidating separate inpatient and outpatient paper-based forms. Submitted referrals are placed directly within a vetting pool for consultant review and subsequent scheduling without the need for rekeying any information (thereby mitigating transcription errors).
Newer endoscopic procedures were built into the e-Referral including endoscopic ultrasound, trans-nasal endoscopy and colon capsules. A nutrition pathway was created to allow transparency of the clinical decision-making leading to the referral for a gastrostomy (PEG) insertion.
The e-Referral incorporated internet links to approved BSG guidelines and easy to understand, prescriptive (and mandatory) rules for the management of patients on anti-coagulants and those proposed for high-risk procedures. Further clinical risk stratification included the mandatory recording of the Glasgow-Blatchford score for patients presenting with suspected GI haemorrhage, and a dashboard was created for the nursing staff to monitor the validation status of such referrals.
The ability to define the define the endoscopist, clinical group or pathway most suitable for the proposed endoscopy allowed downstream targeting of specialist lists. These workstreams facilitated the creation of novel therapeutic lists (for polypectomies <2cm) and bronchoscopy at the weekend thereby augmenting specialist endoscopic capacity.
The nursing care pathway has been completely digitalised from pre-assessment to the subsequent stages of admission, procedure and discharge. This has transformed the quality and standardisation of the nursing documentation, lending particular oversight to the telephone-based pre-assessment service.
Clinical engagement with the Gastroenterologists combined with a departmental review of job plans have meant that there is now a weekly dedicated consultant to validate all endoscopy referrals electronically, including all Trust referrals and those emanating from primary care (via the Direct Access pathway).
Finally, the introduction of an electronic prescribing system has led to a Trust-wide standardisation of the prescription of bowel prep. The use of the protocols within this platform means that prescribing bowel prep is coherent with departmental and national protocols.
What were the outcomes?
Since the root and branch transformation of the department, we now offer an endoscopy service in which all referrals are digital (save for those from primary care), all referrals are validated by a dedicated consultant, all nursing documentation is electronic, and there is an administrative process that is paper-free and flexible to the prevailing demands placed upon it, as evidenced by the creation of additional weekend capacity for specialist lists. There is standardisation of bowel prep regimes and strict adherence to BSG guidelines, particularly those relating to continuing or stopping anti-coagulants.
Objectively, we have seen an improvement in our waiting lists (Figure 1), a reduction in our DNA rates from 7.1% to 3%, and a dramatic fall in our breaching patients from 353 to 12. Our standing within the firmament of regional hospitals within South Yorkshire means that we now are the best performing Trust with regards to waiting lists.
Ongoing prospective audits are evaluating the impact of these interventions on quality assurance, resource utilisation and user satisfaction, with initial indications showing positive outcomes in all areas.
Finally, our recent JAG revalidation awarded the department with the rare accolade of an unconditional pass on the day of inspection.
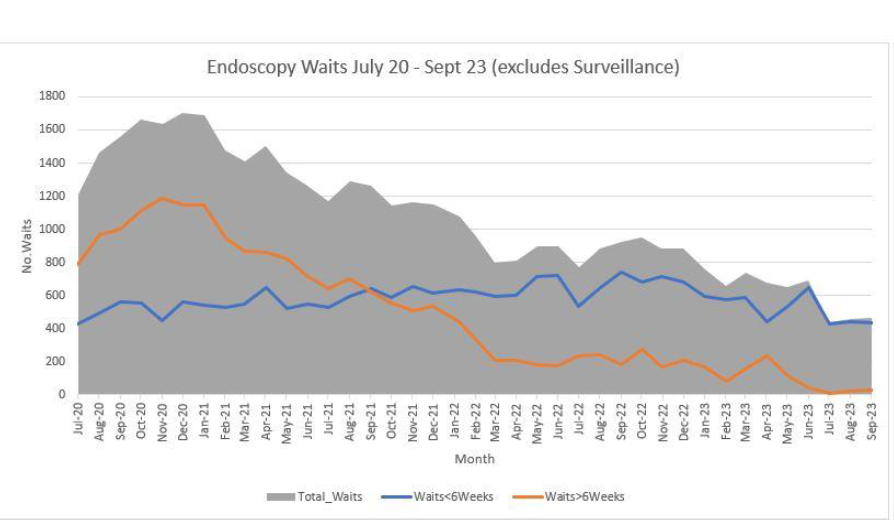
Figure 1.
What were the learning points?
- A transformation of this scale within an endoscopy department requires a multi-disciplinary approach utilising all of the combined experience within the team.
- The use of innovative and bespoke digital pathways ensures the integrity of the clinical dataset, affords transparency of the referral process and facilitates the imposition of mandatory data fields so that critical information is not missed.
- The central focus of the development of the e-Referral was one of being faithful to the BSG and JAG guidelines thereby providing clinical assurance, standardisation of care, improved patient experience and an enhanced approach to patient safety.
- Improvements and iterations in all aspects of the clinical and administrative processes in Endoscopy leads to tangible benefits in terms of list utilisation, DNA’s and waiting list targets.
Read More

